The glucose tolerance test (GTT) is a crucial diagnostic tool used to evaluate how well the body metabolizes glucose. It is particularly important for diagnosing diabetes and prediabetes. The 3-hour glucose tolerance test involves measuring blood sugar levels at various intervals after consuming a glucose-rich drink. This article will delve into what constitutes normal glucose levels during the 3-hour test, how the test is conducted, and its implications for diagnosing diabetes and managing blood sugar levels.
Understanding Glucose Metabolism
To understand the significance of the glucose tolerance test, it is essential to grasp how glucose metabolism works. When we consume carbohydrates, our bodies break them down into glucose, which enters the bloodstream. The pancreas then releases insulin, a hormone that helps cells absorb glucose for energy. If this process is impaired, it can lead to elevated blood sugar levels, which may indicate diabetes or prediabetes.
The Role of Insulin
Insulin plays a vital role in regulating blood glucose levels. Here’s how it works:
Glucose Uptake: Insulin allows cells in the body, particularly muscle and fat cells, to take in glucose from the bloodstream.
Liver Function: Insulin also signals the liver to store excess glucose as glycogen for later use.
Regulating Blood Sugar Levels: When glucose levels are high, insulin helps lower them; when glucose levels drop, glucagon (another hormone) signals the liver to release stored glucose.
When this balance is disrupted, it can result in consistently high blood sugar levels, leading to diabetes.
What is the 3-Hour Glucose Tolerance Test?
The 3-hour glucose tolerance test is an extended version of the standard 2-hour GTT. It assesses how well the body handles a glucose load over an extended period. This test is particularly useful for diagnosing gestational diabetes and identifying insulin resistance in individuals who may be at risk of developing type 2 diabetes.
Procedure of the 3-Hour GTT
The test typically involves the following steps:
Preparation: Patients are advised to fast overnight for at least 8 hours before the test. This means no food or drink except water.
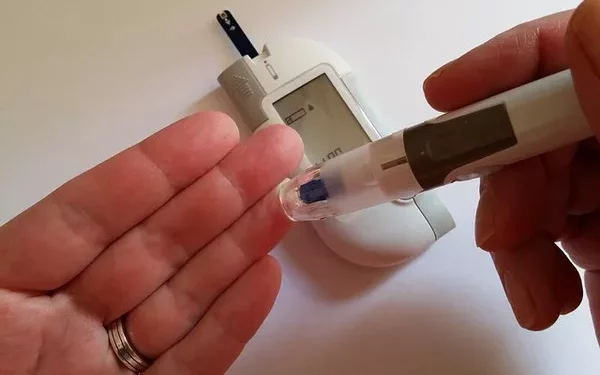
Initial Blood Draw: A baseline blood sample is taken to measure fasting blood glucose levels.
Glucose Consumption: After the baseline measurement, patients are given a glucose solution to drink, typically containing 75 grams of glucose.
Subsequent Blood Draws: Blood samples are taken at regular intervals—usually at 30 minutes, 1 hour, 2 hours, and 3 hours after consuming the glucose solution.
The test measures how effectively the body processes the glucose load over time.
Normal Glucose Levels During the 3-Hour Test
Understanding the expected normal glucose levels during the 3-hour GTT is crucial for interpreting the results. The American Diabetes Association (ADA) provides the following guidelines for normal glucose levels during the test:
Fasting Glucose Level
Normal: Less than 100 mg/dL (5.6 mmol/L)
Prediabetes: 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher
1-Hour Glucose Level
Normal: Less than 180 mg/dL (10.0 mmol/L)
Prediabetes/Diabetes: 180 mg/dL (10.0 mmol/L) or higher
2-Hour Glucose Level
Normal: Less than 140 mg/dL (7.8 mmol/L)
Prediabetes: 140 to 199 mg/dL (7.8 to 11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
3-Hour Glucose Level
Normal: Less than 140 mg/dL (7.8 mmol/L)
Prediabetes: 140 to 199 mg/dL (7.8 to 11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
Interpreting the Results of the 3-Hour GTT
The results of the 3-hour GTT help to determine how well the body metabolizes glucose over time. Here’s how to interpret the results:
1. Normal Glucose Tolerance
If all blood glucose levels remain within the normal ranges throughout the test, the individual is likely to have normal glucose tolerance. This indicates that the body effectively processes glucose.
2. Impaired Glucose Tolerance (Prediabetes)
If the 2-hour or 3-hour glucose levels fall into the prediabetes range, this indicates impaired glucose tolerance. Individuals with prediabetes are at higher risk of developing type 2 diabetes. Lifestyle changes, including dietary modifications and increased physical activity, can help prevent the progression to diabetes.
3. Diabetes Diagnosis
If any of the blood glucose levels during the test meet or exceed the diabetes threshold, a diagnosis of diabetes may be made. This diagnosis may warrant further testing and monitoring, including regular blood glucose checks and possibly insulin therapy.
4. Gestational Diabetes
The 3-hour GTT is also used to diagnose gestational diabetes in pregnant women. If glucose levels are elevated, appropriate interventions can be implemented to ensure the health of both the mother and the baby.
Factors Affecting Glucose Levels During the Test
Several factors can influence the outcomes of the 3-hour glucose tolerance test, including:
1. Diet Prior to the Test
What an individual eats leading up to the test can significantly affect glucose levels. High carbohydrate intake before the test may result in higher baseline glucose levels.
2. Stress Levels
Stress can lead to increased cortisol levels, which can raise blood sugar levels. It is essential to minimize stress leading up to and during the test.
3. Illness
Current illnesses or infections can impact blood glucose levels, potentially leading to inaccurate test results.
4. Medications
Certain medications, such as corticosteroids and some antihypertensives, can affect glucose metabolism and should be discussed with a healthcare provider before the test.
5. Physical Activity
Recent physical activity can lower blood sugar levels, while a lack of activity may lead to higher levels. Patients should follow the provider’s instructions regarding activity levels before the test.
Post-Test Considerations and Next Steps
After completing the 3-hour glucose tolerance test, individuals should review their results with their healthcare provider. Here are some considerations and potential next steps:
1. Understanding Your Results
It’s crucial to understand what the results mean for your health. If diagnosed with prediabetes or diabetes, discussing the implications and necessary lifestyle changes is essential.
2. Developing a Management Plan
If results indicate impaired glucose tolerance or diabetes, healthcare providers can help develop a management plan tailored to the individual. This plan may include:
Dietary Changes: Adopting a balanced diet rich in whole grains, lean proteins, fruits, and vegetables can help manage blood sugar levels.
Regular Monitoring: For individuals diagnosed with diabetes, frequent blood glucose monitoring is critical to maintaining optimal control.
Physical Activity: Incorporating regular exercise into daily routines can help improve insulin sensitivity and lower blood sugar levels.
3. Education and Support
Education on diabetes management, including how to read nutrition labels, manage stress, and recognize the signs of high or low blood sugar, can empower individuals to take control of their health. Joining support groups or diabetes education programs can provide valuable resources and encouragement.
4. Regular Follow-Up
Regular follow-up appointments with healthcare providers are essential for monitoring progress and making necessary adjustments to management plans.
Conclusion
The 3-hour glucose tolerance test is a vital tool for diagnosing diabetes and assessing glucose metabolism. Understanding the normal glucose levels throughout the test is crucial for interpreting results and making informed health decisions.
Normal fasting glucose levels should be less than 100 mg/dL, with subsequent measurements ideally remaining below 140 mg/dL at 2 hours and 3 hours after glucose consumption. Abnormal results can indicate impaired glucose tolerance or diabetes, necessitating further evaluation and management.
Maintaining awareness of factors that influence blood glucose levels and engaging in proactive management strategies can significantly improve health outcomes for individuals at risk of or living with diabetes. By focusing on lifestyle changes, education, and regular monitoring, individuals can take charge of their diabetes management and lead healthier lives.
Related topics:
When Should Type 2 Diabetics Check Blood Sugar?