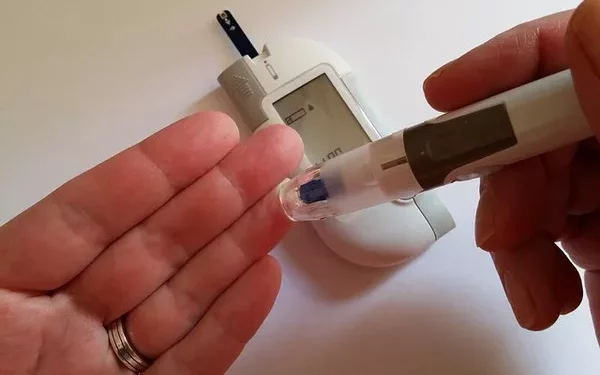
For people with diabetes, exercise is an essential component of managing blood sugar levels and overall health. However, knowing when to check your blood sugar in relation to exercise is crucial for avoiding both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Both can occur before, during, or after exercise, depending on several factors like the intensity of the activity, the type of diabetes you have, and the medications you’re taking.
In this comprehensive article, we’ll delve into the timing of blood sugar checks before and after exercise, why it’s important, and how to adjust your exercise routine based on your blood sugar readings.
Why Is Monitoring Blood Sugar After Exercise Important?
Exercise has a direct impact on blood sugar levels, but the effect can vary depending on the type of physical activity, the duration, and the intensity. When you exercise, your muscles use glucose (sugar) for energy, which can cause your blood sugar levels to drop. In people with Type 1 and Type 2 diabetes, this can lead to hypoglycemia, especially if insulin or other diabetes medications are used.
Conversely, for some people—especially those with Type 2 diabetes—exercise can temporarily raise blood sugar levels due to stress hormones like cortisol. Therefore, monitoring blood sugar after exercise helps you understand how your body responds to different types of activity and allows you to make necessary adjustments to your routine, diet, or medication.
How Does Exercise Affect Blood Sugar Levels?
During Exercise
During physical activity, muscles use glucose for energy, which lowers the blood sugar level. For people with diabetes, this can be beneficial as it improves insulin sensitivity and helps regulate blood sugar over time. However, for those on insulin or certain medications like sulfonylureas, exercise increases the risk of hypoglycemia.
After Exercise
The effect of exercise on blood sugar can last for hours, or even up to 24 hours. After exercise, muscles continue to absorb glucose from the bloodstream, which can lead to a gradual drop in blood sugar. This is why it’s important to monitor blood sugar not just immediately after exercise, but several hours later as well, to avoid delayed hypoglycemia.
When Should You Check Your Blood Sugar After Exercise?
Immediately After Exercise
Checking your blood sugar immediately after exercising provides immediate feedback on how your body responded to the workout. This is particularly important if you are on insulin or medication that can cause hypoglycemia. If your blood sugar drops too low, you may need to consume fast-acting carbohydrates to prevent a hypoglycemic episode.
What to look for: A blood sugar level below 70 mg/dL indicates hypoglycemia. If your blood sugar is low, consume 15 grams of fast-acting carbohydrates (e.g., glucose tablets, fruit juice) and recheck your blood sugar after 15 minutes.
What if it’s high? If your blood sugar is high after exercise, it may indicate that the intensity of the workout was too much or that your insulin sensitivity was affected. High-intensity exercise can trigger stress hormones, which in turn raise blood sugar levels temporarily. In this case, it’s important to monitor your blood sugar over the next few hours and adjust your insulin or medication as needed, with guidance from your healthcare provider.
One to Two Hours After Exercise
Checking your blood sugar 1-2 hours after exercise can help you detect delayed hypoglycemia. Some people with diabetes experience a drop in blood sugar several hours after exercising, particularly if the workout was intense or prolonged. This is because muscles continue to take up glucose to replenish energy stores after exercise.
What to look for: A blood sugar reading that continues to drop within 1-2 hours after exercise might suggest you are at risk for delayed hypoglycemia. If your blood sugar is lower than 100 mg/dL, consider eating a snack with protein and carbohydrates to stabilize your levels.
Why it’s important: Delayed hypoglycemia can occur as long as 24 hours after exercise, particularly after vigorous or prolonged physical activity. Monitoring at this time helps ensure your blood sugar remains stable, reducing the risk of a sudden drop later in the day or even overnight.
Four to Six Hours After Exercise
Checking your blood sugar 4-6 hours after exercise helps you track the longer-term effects of physical activity on your glucose levels. For many people with diabetes, blood sugar continues to decrease during this window due to the muscles’ ongoing use of glucose for energy replenishment.
What to look for: If your blood sugar has dropped since your earlier readings, you may need to adjust your post-exercise meal or medication. On the other hand, if your blood sugar remains elevated, you may want to discuss changes to your medication or insulin regimen with your healthcare provider.
Overnight Monitoring
For people who exercise late in the day, it’s important to check blood sugar before bed and possibly during the night, particularly after intense exercise. Nighttime hypoglycemia can be dangerous, and blood sugar levels can drop unexpectedly during sleep.
What to look for: If your blood sugar is lower than usual before bed, eat a small snack that includes protein and carbohydrates to prevent nighttime hypoglycemia. In some cases, you may need to adjust your nighttime insulin dose, but this should be done under the supervision of your healthcare provider.
How to Adjust Your Blood Sugar Monitoring Based on Exercise Type
Different types of exercise have varying effects on blood sugar levels. It’s essential to adjust your monitoring routine depending on the type of activity you’re doing.
Aerobic Exercise
Aerobic activities like walking, jogging, cycling, or swimming tend to lower blood sugar levels during and after exercise. These exercises help improve insulin sensitivity, which means your body uses glucose more efficiently.
Monitoring recommendation: Check blood sugar before, immediately after, and 1-2 hours after aerobic exercise. If you’re doing long-duration aerobic exercise, such as a marathon or long-distance cycling, consider checking your blood sugar during the workout as well to avoid hypoglycemia.
Strength Training
Strength training or resistance exercises can have a mixed effect on blood sugar. Initially, blood sugar may rise slightly due to the stress hormone response, but it typically drops afterward as muscles take up glucose.
Monitoring recommendation: Check blood sugar immediately after strength training and 1-2 hours later. Monitor for delayed hypoglycemia, especially if your workout was intense or involved large muscle groups.
High-Intensity Interval Training (HIIT)
HIIT workouts are known to cause a temporary rise in blood sugar due to the release of stress hormones. However, after the workout, blood sugar levels often drop as your muscles replenish their energy stores.
Monitoring recommendation: Check blood sugar before, immediately after, and 1-2 hours after a HIIT workout. Be aware of potential delayed hypoglycemia, especially several hours later or overnight.
Factors That Influence Post-Exercise Blood Sugar Levels
1. Insulin and Medications
For people with diabetes, the type of insulin or medications they take can significantly impact how their blood sugar behaves after exercise. Rapid-acting insulins, sulfonylureas, and meglitinides can increase the risk of hypoglycemia during or after exercise.
Tip: Always check your blood sugar before exercise, especially if you take insulin. You may need to adjust your insulin dose or eat a snack before exercising to avoid hypoglycemia.
2. Time of Day
Blood sugar levels can fluctuate depending on the time of day. For example, morning exercise may result in different blood sugar patterns than evening exercise due to variations in hormone levels like cortisol and insulin sensitivity.
Tip: Monitor how your body responds to exercise at different times of the day and adjust your blood sugar checks accordingly.
3. Duration and Intensity of Exercise
Longer or more intense workouts tend to have a greater impact on blood sugar levels. Vigorous exercise can increase the risk of delayed hypoglycemia for up to 24 hours post-exercise.
Tip: For long or intense workouts, monitor your blood sugar more frequently, particularly 4-6 hours post-exercise and before bed.
4. Food Intake
What you eat before and after exercise can also affect your blood sugar levels. A meal high in carbohydrates may raise your blood sugar initially, while a balanced meal with protein and fat can help stabilize it.
Tip: Pay attention to your meal timing and composition. You may need to adjust your food intake to support stable blood sugar levels during and after exercise.
How to Prevent Hypoglycemia After Exercise
Hypoglycemia after exercise is a common concern for people with diabetes, particularly those taking insulin or certain medications. Here are some strategies to prevent low blood sugar after exercise:
1. Eat a Snack Before or After Exercise
A small snack that includes carbohydrates and protein can help prevent hypoglycemia during and after exercise. Good options include an apple with peanut butter, a yogurt with berries, or a small granola bar.
2. Adjust Your Insulin or Medication
If you’re at risk for exercise-induced hypoglycemia, your healthcare provider may recommend adjusting your insulin dose or medication on days when you exercise. Always discuss any changes with your doctor before making adjustments.
3. Stay Hydrated
Dehydration can exacerbate blood sugar fluctuations. Make sure you’re drinking enough water before, during, and after exercise to keep your blood sugar stable.
4. Monitor Regularly
Frequent monitoring is the best way to prevent hypoglycemia. Checking your blood sugar at multiple points before, during, and after exercise allows you to respond quickly to any changes.
See also: What is the Normal Fasting Blood Sugar (FBS) Result?
Conclusion: Timing is Key to Managing Blood Sugar After Exercise
Monitoring your blood sugar after exercise is crucial for preventing both hypoglycemia and hyperglycemia. It’s recommended to check your blood sugar immediately after exercise, 1-2 hours later, and possibly again 4-6 hours after, especially if your workout was intense. The timing and frequency of your checks should be adjusted based on the type of exercise, the medications you take, and how your body typically responds to physical activity.
By understanding your unique patterns, you can make informed decisions about your exercise routine, diet, and medication, ensuring that you maintain optimal blood sugar levels and avoid complications. Always consult your healthcare provider for personalized advice on managing blood sugar with exercise.
Related topics: