Hyperglycemia, or high blood sugar, is a common condition among people with diabetes, but it can occur in anyone due to various factors. When blood glucose levels rise above normal, it can lead to serious complications if not managed promptly. Understanding how to recognize and treat hyperglycemia is crucial for maintaining health and preventing emergencies. This article explores the causes of hyperglycemia, its symptoms, emergency treatments, and strategies for prevention.
Understanding Hyperglycemia
Hyperglycemia occurs when there is an excess of glucose in the bloodstream. This condition can arise from various factors, including inadequate insulin production, insulin resistance, excessive carbohydrate intake, stress, and certain medications. Chronic hyperglycemia can lead to complications such as diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS), both of which require immediate medical intervention.
1. Definition of Hyperglycemia
Hyperglycemia is defined as a blood glucose level above the normal range. The American Diabetes Association (ADA) defines hyperglycemia as a fasting blood glucose level of 126 mg/dL or higher and a postprandial (after eating) level of 180 mg/dL or higher.
2. Causes of Hyperglycemia
Several factors can contribute to hyperglycemia:
Inadequate Insulin Production: This is common in individuals with type 1 diabetes, where the pancreas does not produce enough insulin.
Insulin Resistance: In type 2 diabetes, the body’s cells become resistant to the effects of insulin, leading to elevated blood sugar levels.
Dietary Choices: Consuming large amounts of carbohydrates or sugary foods can raise blood glucose levels significantly.
Stress: Physical or emotional stress can cause the release of hormones that raise blood sugar levels.
Illness or Infection: Conditions such as infections or illnesses can elevate blood sugar levels due to stress responses in the body.
Medications: Certain medications, including corticosteroids and some diuretics, can raise blood sugar levels.
Symptoms of Hyperglycemia
Recognizing the symptoms of hyperglycemia is crucial for early intervention. Symptoms may vary based on the severity and duration of elevated blood glucose levels:
Frequent Urination (Polyuria): High blood sugar levels can cause the kidneys to excrete more glucose, leading to increased urination.
Increased Thirst (Polydipsia): As the body loses more fluid through urination, thirst increases to compensate for the lost fluids.
Fatigue: Elevated blood sugar levels can cause fatigue and weakness due to the body’s inability to utilize glucose effectively for energy.
Blurred Vision: High glucose levels can lead to swelling in the lenses of the eyes, affecting vision.
Headaches: Hyperglycemia can cause headaches and difficulty concentrating.
Dry Mouth and Skin: Dehydration from excessive urination can lead to a dry mouth and skin.
Unexplained Weight Loss: In some cases, the body starts to break down fat and muscle for energy, leading to weight loss.
Emergency Situations Related to Hyperglycemia
Hyperglycemia can progress to severe complications, requiring immediate medical attention. Two critical conditions associated with uncontrolled hyperglycemia are:
1. Diabetic Ketoacidosis (DKA)
DKA is a serious condition that primarily affects individuals with type 1 diabetes. It occurs when the body starts breaking down fat for energy instead of glucose, leading to the production of ketones. High levels of ketones can lead to acidosis, a dangerous condition that requires emergency treatment.
Symptoms of DKA:
- Nausea and vomiting
- Abdominal pain
- Rapid breathing (Kussmaul respiration)
- Fruity-scented breath
- Confusion or altered mental status
- Weakness or fatigue
2. Hyperglycemic Hyperosmolar State (HHS)
HHS is more common in individuals with type 2 diabetes and is characterized by extremely high blood sugar levels without significant ketone production. It leads to severe dehydration and can result in coma or death if untreated.
Symptoms of HHS:
- Extreme thirst
- High blood sugar levels (often exceeding 600 mg/dL)
- Dry mouth and skin
- Confusion or lethargy
- Seizures
Emergency Treatment for Hyperglycemia
The treatment of hyperglycemia, especially in emergency situations like DKA or HHS, requires prompt intervention to prevent serious complications. The following steps outline emergency treatment protocols.
1. Call for Help
In an emergency, it is crucial to seek immediate medical assistance. If symptoms of severe hyperglycemia, DKA, or HHS occur, call emergency services or have someone take the person to the hospital.
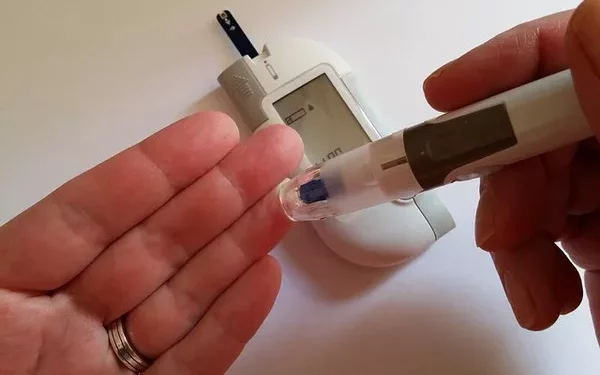
2. Monitor Blood Sugar Levels
If the individual has access to a glucose meter, checking blood sugar levels is essential. This helps determine the severity of hyperglycemia and guides treatment decisions.
Mild Hyperglycemia: Blood sugar levels between 180-250 mg/dL may be managed at home with appropriate interventions.
Moderate to Severe Hyperglycemia: Blood sugar levels above 250 mg/dL, especially with symptoms of DKA or HHS, require immediate medical attention.
3. Administer Insulin
In cases of severe hyperglycemia, particularly with DKA or HHS, insulin administration is a critical component of treatment:
Insulin Protocol: In a medical setting, intravenous (IV) insulin may be administered to rapidly reduce blood glucose levels. For individuals with DKA, initial boluses of insulin may be followed by a continuous infusion.
Subcutaneous Insulin: If an individual is conscious and able to eat, subcutaneous insulin may be administered if prescribed. It is essential to follow a healthcare provider’s instructions regarding dosages.
4. Hydration
Rehydration is a vital component of emergency treatment:
IV Fluids: Individuals with DKA or HHS typically require IV fluids to rehydrate and correct electrolyte imbalances. Normal saline is often administered initially, followed by a switch to D5W (5% dextrose in water) once blood sugar levels decrease.
Monitoring Electrolytes: Potassium levels may drop as insulin lowers blood glucose levels. Therefore, monitoring and replacing electrolytes, particularly potassium, is essential during treatment.
5. Electrolyte Management
Electrolyte imbalances can occur with hyperglycemia and must be managed carefully:
Potassium Levels: Hypokalemia (low potassium levels) can occur due to insulin therapy. Regular monitoring of potassium levels is necessary, and potassium replacement may be needed.
Sodium and Chloride Levels: Monitoring sodium and chloride levels is also essential to ensure electrolyte balance.
6. Identify Underlying Causes
Identifying and addressing the underlying causes of hyperglycemia is crucial for effective management:
Illness or Infection: Treat any underlying infections or illnesses contributing to hyperglycemia.
Medication Adjustments: Review and adjust any medications that may be impacting blood sugar levels.
Post-Emergency Care and Management
After emergency treatment for hyperglycemia, ongoing management is essential to prevent future episodes. The following strategies can help individuals manage their blood sugar levels effectively.
1. Develop an Individualized Treatment Plan
Work with healthcare providers to create a personalized treatment plan that includes:
Insulin Therapy: Adjust insulin regimens as needed to manage blood sugar levels effectively.
Oral Medications: For those with type 2 diabetes, review oral medications that may help control blood sugar levels.
2. Monitor Blood Sugar Regularly
Regular blood glucose monitoring is essential for managing diabetes and preventing hyperglycemia:
Frequency of Monitoring: Monitor blood sugar levels multiple times a day, especially during periods of illness or stress.
Record Keeping: Keep a log of blood sugar readings to identify patterns and discuss them with healthcare providers.
3. Adjust Diet and Nutrition
Diet plays a crucial role in managing blood sugar levels:
Balanced Meals: Incorporate a balanced diet rich in whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables.
Carbohydrate Counting: Learn to count carbohydrates and make informed choices about portion sizes.
4. Stay Active
Regular physical activity can help improve insulin sensitivity and regulate blood sugar levels:
Exercise Routine: Aim for at least 150 minutes of moderate-intensity exercise each week. This can include walking, cycling, swimming, or other activities that raise the heart rate.
Consistency: Establish a consistent exercise routine to help maintain healthy blood sugar levels.
5. Manage Stress
Stress can impact blood sugar levels, making stress management techniques important:
Mindfulness and Relaxation: Incorporate relaxation techniques, such as deep breathing exercises, meditation, or yoga, to help manage stress.
Adequate Sleep: Prioritize getting enough sleep, as poor sleep can affect blood sugar regulation.
6. Regular Check-Ups
Routine medical check-ups are essential for monitoring diabetes management:
Annual Examinations: Schedule regular check-ups with healthcare providers to assess blood sugar control and adjust treatment plans as needed.
Screen for Complications: Regular screenings for diabetes-related complications, such as eye exams, kidney function tests, and foot examinations, are vital for maintaining health.
See also: Does Hyperglycemia Cause Vomiting?
Conclusion
Hyperglycemia is a serious condition that requires immediate attention, especially when it progresses to complications such as DKA or HHS. Recognizing the symptoms, understanding the emergency treatment protocols, and implementing preventive measures are essential for managing blood sugar levels effectively. Individuals with diabetes must work closely with healthcare providers to develop personalized treatment plans that include monitoring, medication management, diet, exercise, and stress management strategies. Early intervention and proactive management can help prevent hyperglycemia and its associated complications, ensuring a healthier and more fulfilling life. If you or someone you know is experiencing symptoms of hyperglycemia, do not hesitate to seek medical help.
Related topics:
How Can I Lower My Hyperglycemia Naturally?