Hyperglycemia, or high blood sugar, is a condition that occurs when there is an excessive amount of glucose in the bloodstream. It is a common issue among people with diabetes and can lead to serious health complications if not managed effectively. In this article, we will explore what constitutes hyperglycemia, the ranges that define it, the underlying causes, symptoms, complications, and the importance of management strategies to maintain healthy blood glucose levels.
What is Hyperglycemia?
Defining Hyperglycemia
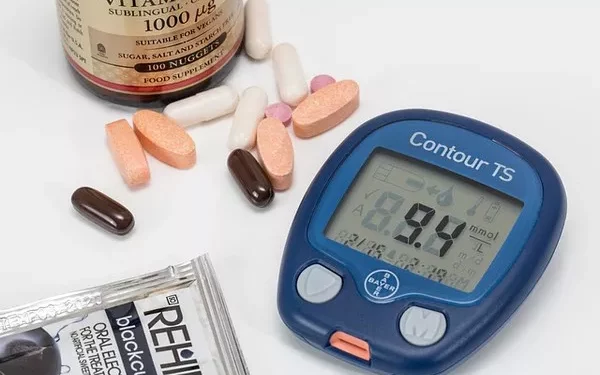
Hyperglycemia occurs when blood glucose levels rise above normal. It is typically defined as having a blood glucose level greater than 130 mg/dL (7.2 mmol/L) when fasting or above 180 mg/dL (10 mmol/L) two hours after eating. However, these thresholds can vary based on individual circumstances, such as whether a person has diabetes and their specific treatment plan.
Normal Blood Glucose Levels
To understand hyperglycemia, it is essential to know what normal blood glucose levels are. According to the American Diabetes Association (ADA), the following ranges are considered normal for adults:
Fasting Blood Glucose: Less than 100 mg/dL (5.6 mmol/L)
Postprandial Blood Glucose (2 hours after eating): Less than 140 mg/dL (7.8 mmol/L)
Hemoglobin A1c (HbA1c): Less than 5.7%
These values provide a reference point to understand when blood sugar levels become elevated.
What Constitutes Hyperglycemia?
Thresholds for Hyperglycemia
Mild Hyperglycemia: Blood glucose levels from 140 to 180 mg/dL (7.8 to 10 mmol/L)
Moderate Hyperglycemia: Blood glucose levels from 180 to 240 mg/dL (10 to 13.3 mmol/L)
Severe Hyperglycemia: Blood glucose levels above 240 mg/dL (13.3 mmol/L)
These thresholds help healthcare providers categorize the severity of hyperglycemia and determine appropriate management strategies.
Chronic Hyperglycemia
Chronic hyperglycemia refers to consistently elevated blood sugar levels over an extended period, often indicated by an HbA1c level above 6.5% (48 mmol/mol). This condition is prevalent in individuals with uncontrolled diabetes and can lead to long-term complications.
Causes of Hyperglycemia
Understanding the underlying causes of hyperglycemia is crucial for effective management. Several factors can contribute to elevated blood sugar levels:
1. Diabetes Mellitus
Type 1 Diabetes: In this condition, the body does not produce insulin, leading to high blood glucose levels. People with Type 1 diabetes require insulin therapy to manage their blood sugar.
Type 2 Diabetes: This form of diabetes occurs when the body becomes resistant to insulin or does not produce enough insulin. Lifestyle factors, such as obesity and physical inactivity, play a significant role in the development of Type 2 diabetes.
2. Stress
Physical or emotional stress can cause the release of hormones such as cortisol and adrenaline, which raise blood glucose levels. Stress can arise from various sources, including illness, injury, or emotional turmoil.
3. Hormonal Changes
Certain hormones, including glucagon and epinephrine, can stimulate the liver to release glucose into the bloodstream, contributing to hyperglycemia. Conditions such as Cushing’s syndrome or hormonal imbalances can exacerbate this effect.
4. Medications
Some medications can cause elevated blood sugar levels. For example:
Corticosteroids: Often used to treat inflammation, these medications can increase blood glucose levels.
Thiazide Diuretics: These can affect glucose metabolism and lead to hyperglycemia.
5. Dietary Choices
Consuming high amounts of carbohydrates or sugary foods can lead to spikes in blood sugar levels, especially in individuals with diabetes who may have difficulty managing their intake.
6. Lack of Physical Activity
Physical inactivity can contribute to weight gain and insulin resistance, both of which increase the likelihood of developing hyperglycemia.
Symptoms of Hyperglycemia
Recognizing the symptoms of hyperglycemia is essential for timely intervention. Common symptoms include:
Increased Thirst (Polydipsia): High blood sugar levels can lead to dehydration, causing excessive thirst.
Frequent Urination (Polyuria): Elevated glucose levels can cause the kidneys to excrete more glucose in the urine, leading to increased urination.
Fatigue: The body may struggle to utilize glucose for energy, resulting in fatigue and weakness.
Blurred Vision: High blood sugar can affect the lens of the eye, leading to temporary changes in vision.
Headaches: Elevated blood glucose can lead to headaches and general discomfort.
Dry Mouth and Skin: Dehydration due to frequent urination can cause dryness in the mouth and skin.
Weight Loss: In cases of uncontrolled diabetes, the body may start breaking down fat and muscle for energy, leading to weight loss.
Severe Symptoms
In severe cases of hyperglycemia, individuals may experience:
Nausea and Vomiting: High blood sugar can lead to a buildup of ketones, causing nausea.
Difficulty Breathing: Rapid breathing or shortness of breath may occur.
Fruity Breath: A distinctive fruity odor on the breath can indicate the presence of ketones.
Confusion or Altered Mental State: Severe hyperglycemia can affect cognitive function.
Complications of Hyperglycemia
If left untreated, hyperglycemia can lead to various acute and chronic complications.
1. Diabetic Ketoacidosis (DKA)
DKA is a life-threatening condition that occurs primarily in individuals with Type 1 diabetes. It results from a severe lack of insulin, leading to the production of ketones. Symptoms include nausea, vomiting, abdominal pain, rapid breathing, and altered consciousness. DKA requires immediate medical attention and often necessitates hospitalization.
2. Hyperglycemic Hyperosmolar State (HHS)
HHS is more common in individuals with Type 2 diabetes and is characterized by extremely high blood sugar levels without significant ketone production. Symptoms include severe dehydration, confusion, and lethargy. HHS is also a medical emergency requiring prompt treatment.
3. Long-Term Complications
Chronic hyperglycemia can lead to long-term complications affecting various organ systems, including:
Cardiovascular Disease: High blood sugar can damage blood vessels, increasing the risk of heart disease and stroke.
Neuropathy: Prolonged elevated glucose levels can damage nerves, leading to numbness, tingling, and pain, particularly in the feet and hands.
Retinopathy: Diabetes can damage the blood vessels in the retina, leading to vision problems and potentially blindness.
Nephropathy: High blood sugar can damage the kidneys, leading to kidney disease and possible kidney failure.
Poor Wound Healing: Hyperglycemia can impair the body’s ability to heal wounds, increasing the risk of infections.
Management of Hyperglycemia
Effective management of hyperglycemia involves a combination of lifestyle changes, medication, and regular monitoring. Here are some strategies:
1. Monitoring Blood Sugar Levels
Regular blood sugar monitoring is crucial for individuals with diabetes. Keeping track of blood glucose levels helps identify patterns and triggers for hyperglycemia, allowing for timely interventions.
2. Healthy Eating
Balanced Diet: Focus on a balanced diet rich in whole foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of refined carbohydrates and sugary foods.
Carbohydrate Counting: Learn to count carbohydrates to better manage blood sugar levels. This is especially important for individuals on insulin therapy.
3. Physical Activity
Regular physical activity plays a significant role in managing blood sugar levels:
Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming.
Incorporate resistance training at least twice a week to build muscle and improve insulin sensitivity.
4. Medication Management
For individuals with diabetes, medication may be necessary to control blood sugar levels. Options include:
Insulin Therapy: Essential for individuals with Type 1 diabetes and may be required for some with Type 2 diabetes.
Oral Medications: Various classes of oral medications can help lower blood sugar levels in Type 2 diabetes.
5. Stress Management
Managing stress is essential for blood sugar control. Techniques such as yoga, meditation, and deep breathing exercises can help reduce stress and improve overall well-being.
6. Regular Check-ups
Regular visits to healthcare providers are vital for monitoring diabetes management and adjusting treatment plans as needed. Routine blood tests, including HbA1c levels, help assess long-term blood sugar control.
See also: How Do You Fix Hyperglycemia?
Conclusion
Hyperglycemia is a serious condition that can lead to acute and chronic complications if left unmanaged. Understanding the ranges that indicate hyperglycemia is essential for effective management. By adopting a healthy lifestyle, monitoring blood sugar levels, and working closely with healthcare providers, individuals can reduce the risk of hyperglycemia and its associated complications. It is crucial for individuals with diabetes to remain vigilant and proactive in managing their blood sugar levels to achieve optimal health and well-being.
Related topics:
Can You Live with Hyperglycemia?