Hypoglycemia, commonly referred to as low blood sugar, is a condition that occurs when the glucose levels in the bloodstream drop below normal levels. While most people associate hypoglycemia with diabetes and insulin use, non-diabetic hypoglycemia can also occur. This article explores the nature of non-diabetic hypoglycemia, its causes, symptoms, diagnosis, and management strategies.
Understanding Hypoglycemia
1. Definition of Hypoglycemia
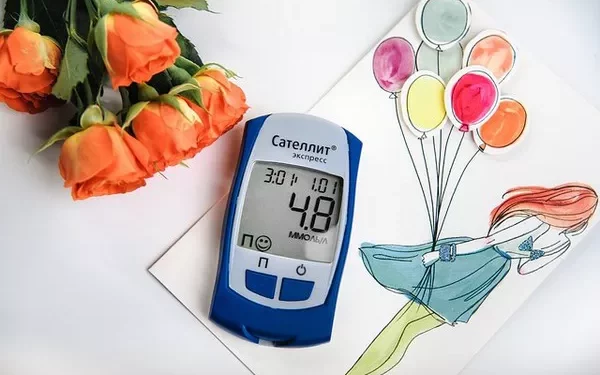
Hypoglycemia is generally defined as a blood glucose level of less than 70 mg/dL (3.9 mmol/L). However, the specific threshold may vary depending on individual circumstances and symptoms. Low blood sugar can lead to various physical and mental health issues, impacting an individual’s quality of life.
2. Types of Hypoglycemia
Hypoglycemia can be classified into two main types:
Diabetic Hypoglycemia: This type occurs in individuals with diabetes, often due to insulin therapy or oral diabetes medications. It results from an imbalance between insulin and glucose levels in the body.
Non-Diabetic Hypoglycemia: This type occurs in individuals without diabetes and can be caused by various factors, including dietary choices, hormonal imbalances, or medical conditions.
What is Non-Diabetic Hypoglycemia?
Non-diabetic hypoglycemia occurs when an individual experiences low blood sugar levels without a diagnosis of diabetes. It can be further categorized into two main types:
1. Reactive Hypoglycemia
Reactive hypoglycemia occurs after eating, usually within 2-4 hours post-meal. This condition often arises when the body produces an excessive amount of insulin in response to a carbohydrate-rich meal. The rapid drop in blood sugar levels can lead to symptoms of hypoglycemia.
2. Fasting Hypoglycemia
Fasting hypoglycemia occurs when an individual experiences low blood sugar levels after prolonged periods without eating. This can happen due to extended fasting, malnutrition, or certain medical conditions.
3. Causes of Non-Diabetic Hypoglycemia
Several factors can contribute to non-diabetic hypoglycemia. These include:
Dietary Choices: Consuming meals high in carbohydrates, especially refined sugars, can trigger reactive hypoglycemia. This is particularly true when meals are followed by a lack of adequate protein and fat.
Hormonal Imbalances: Hormonal deficiencies, such as adrenal insufficiency or growth hormone deficiency, can affect glucose regulation.
Alcohol Consumption: Drinking alcohol, especially on an empty stomach, can interfere with glucose production in the liver, leading to low blood sugar.
Medications: Certain medications, including some antibiotics and those used to treat malaria, can cause hypoglycemia as a side effect.
Medical Conditions: Some medical conditions, such as insulinomas (insulin-producing tumors), liver disease, and severe infections, can also result in non-diabetic hypoglycemia.
Hormonal Disorders: Conditions that affect hormone levels, such as adrenal insufficiency, can impair the body’s ability to manage blood sugar levels effectively.
Excessive Exercise: Intense physical activity can lead to low blood sugar levels, especially if not paired with adequate nutrition.
Symptoms of Non-Diabetic Hypoglycemia
The symptoms of non-diabetic hypoglycemia can vary among individuals. Common symptoms include:
1. Early Symptoms
Shakiness: A feeling of trembling or shakiness in the body.
Sweating: Increased perspiration, often experienced even when not physically active.
Nervousness: Feelings of anxiety or nervousness that can accompany low blood sugar.
Heart Palpitations: An increase in heart rate or a feeling of fluttering in the chest.
Hunger: A strong feeling of hunger, which can be an early sign of low blood sugar.
Dizziness: Lightheadedness or feeling faint can occur when blood sugar levels drop.
2. Severe Symptoms
If hypoglycemia is not addressed, symptoms can worsen and may include:
Confusion: Difficulty thinking clearly or concentrating.
Irritability: Increased moodiness or irritability can occur during hypoglycemic episodes.
Fatigue: A general feeling of tiredness and lack of energy.
Blurred Vision: Changes in vision, such as blurriness or double vision.
Seizures: In extreme cases, hypoglycemia can lead to seizures or loss of consciousness.
3. Long-Term Effects
Repeated episodes of hypoglycemia can lead to hypoglycemia unawareness, a condition where individuals no longer recognize the early symptoms of low blood sugar. This can increase the risk of severe hypoglycemic events.
Diagnosing Non-Diabetic Hypoglycemia
Diagnosing non-diabetic hypoglycemia involves a thorough assessment of symptoms, dietary habits, and blood glucose levels. Healthcare providers may utilize several methods to confirm the diagnosis.
1. Patient History and Symptom Review
A detailed medical history and symptom review are crucial. Patients should provide information about:
- The frequency and timing of symptoms
- Dietary habits and recent food intake
- Any medications currently being taken
2. Blood Glucose Monitoring
Blood glucose levels are monitored during suspected hypoglycemic episodes. This can be done through:
Fingerstick Testing: A quick test to measure blood sugar levels at home or in a clinical setting.
Continuous Glucose Monitoring (CGM): A device worn on the body that continuously measures glucose levels, providing valuable data over time.
3. Oral Glucose Tolerance Test (OGTT)
In some cases, an oral glucose tolerance test may be conducted. This test involves measuring blood glucose levels at intervals after consuming a glucose-rich drink. Abnormal results may indicate reactive hypoglycemia.
4. Laboratory Tests
Healthcare providers may order additional laboratory tests to rule out underlying conditions, such as hormonal deficiencies or other metabolic disorders.
Management Strategies for Non-Diabetic Hypoglycemia
Managing non-diabetic hypoglycemia involves a combination of dietary adjustments, lifestyle changes, and medical interventions. The goal is to prevent low blood sugar episodes and maintain stable glucose levels.
1. Dietary Management
Balanced Meals: Focus on consuming balanced meals that include complex carbohydrates, protein, and healthy fats. This combination helps regulate blood sugar levels and prevent rapid fluctuations.
Frequent Small Meals: Eating smaller, more frequent meals can help maintain stable blood sugar levels throughout the day. Aim for five to six small meals instead of three large ones.
Limit Sugary Foods: Avoid foods high in refined sugars, as they can cause rapid spikes and subsequent drops in blood sugar levels. Opt for whole grains, fruits, and vegetables instead.
Include Protein and Fiber: Incorporating protein and fiber into meals can slow down the absorption of carbohydrates, helping to prevent reactive hypoglycemia.
2. Lifestyle Modifications
Exercise: Regular physical activity is important for overall health but should be balanced with dietary intake. Avoid excessive or prolonged exercise without proper nutrition.
Avoid Alcohol on an Empty Stomach: If consuming alcohol, do so with food to help prevent low blood sugar levels.
Monitor Blood Sugar Levels: Regular monitoring can help individuals identify patterns and take preventive actions to avoid hypoglycemia.
3. Medical Interventions
If dietary and lifestyle changes are insufficient, healthcare providers may consider additional medical interventions:
Medications: In some cases, medications may be prescribed to help regulate blood sugar levels. For example, medications that influence insulin secretion may be considered.
Hormonal Therapy: For individuals with hormonal deficiencies, hormone replacement therapy may be appropriate to help manage blood sugar levels.
4. Education and Support
Education is crucial for individuals with non-diabetic hypoglycemia. Understanding the condition, its triggers, and management strategies can empower individuals to take control of their health. Support groups and resources can provide additional guidance and encouragement.
When to Seek Medical Attention
While mild hypoglycemic episodes can often be managed at home, individuals should seek medical attention in the following situations:
Severe Symptoms: If experiencing severe symptoms such as confusion, seizures, or loss of consciousness, immediate medical assistance is necessary.
Frequent Episodes: If hypoglycemic episodes occur frequently or without clear triggers, it is essential to consult a healthcare provider for further evaluation.
Underlying Health Issues: Individuals with underlying health conditions or concerns about their blood sugar levels should seek medical advice to ensure appropriate management.
See also: What You Should Do for Hypoglycemia
Conclusion
Non-diabetic hypoglycemia is a condition that can significantly impact an individual’s quality of life. Understanding its causes, symptoms, and management strategies is essential for preventing and addressing low blood sugar episodes. By implementing dietary changes, lifestyle modifications, and working closely with healthcare providers, individuals can take proactive steps toward managing non-diabetic hypoglycemia effectively.
If you experience symptoms of hypoglycemia, it’s important to consult with a healthcare professional for a proper diagnosis and tailored management plan. By maintaining awareness and taking preventive measures, individuals can enjoy a healthier, more balanced life.
Related topics:
What Can Hypoglycemia Lead To?