Fasting blood glucose levels are a critical indicator of metabolic health and a cornerstone in diagnosing and managing diabetes. Understanding what constitutes a normal fasting glucose level is essential for maintaining overall health and preventing diabetes-related complications. This comprehensive article will explore the concept of fasting glucose, factors affecting it, normal ranges, and the implications of abnormal levels.
Understanding Fasting Glucose
What is Fasting Glucose?
Fasting glucose refers to the blood sugar level measured after a period of fasting, typically for at least 8 hours. This measurement provides insight into how well the body regulates blood sugar levels without the influence of recent food intake. It is a key metric used in both diagnosing diabetes and monitoring glucose management in individuals with diabetes.
Why is Fasting Glucose Important?
Fasting glucose levels are important for several reasons:
Diagnosis of Diabetes: Abnormal fasting glucose levels are used to diagnose diabetes and prediabetes.
Monitoring Glycemic Control: Regular fasting glucose measurements help individuals with diabetes assess their blood sugar control.
Assessing Insulin Sensitivity: Fasting glucose levels can indicate how effectively the body uses insulin.
Normal Fasting Glucose Levels
Standard Reference Ranges
The American Diabetes Association (ADA) and other health organizations provide guidelines for normal fasting glucose levels. The standard reference ranges are:
Normal: Fasting blood glucose levels less than 100 mg/dL (5.6 mmol/L).
Prediabetes: Fasting blood glucose levels between 100 and 125 mg/dL (5.6 to 6.9 mmol/L).
Diabetes: Fasting blood glucose levels of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions.
Interpreting the Results
Normal Range: Individuals with fasting glucose levels less than 100 mg/dL are generally considered to have normal glucose metabolism.
Prediabetes: Levels between 100 and 125 mg/dL suggest an increased risk of developing diabetes, known as prediabetes. Lifestyle modifications are often recommended to prevent progression.
Diabetes: Levels of 126 mg/dL or higher indicate a diagnosis of diabetes. Further tests and evaluations are typically conducted to confirm the diagnosis and assess treatment options.
Factors Affecting Fasting Glucose Levels
1. Diet
Diet plays a significant role in fasting glucose levels. Certain foods can impact glucose metabolism and insulin sensitivity:
Carbohydrate Intake: High carbohydrate diets, particularly those with refined sugars, can lead to increased fasting glucose levels.
Glycemic Index: Foods with a high glycemic index (GI) can cause rapid spikes in blood sugar levels.
Meal Timing: Irregular eating patterns or late-night meals can influence fasting glucose levels.
2. Physical Activity
Regular physical activity helps improve insulin sensitivity and regulate blood glucose levels. Sedentary behavior, on the other hand, can contribute to higher fasting glucose levels and increased risk of diabetes.
3. Stress
Stress can affect glucose metabolism by increasing the production of stress hormones like cortisol. Elevated cortisol levels can lead to increased blood glucose levels.
4. Medications
Certain medications can impact fasting glucose levels:
Steroids: Corticosteroids can increase blood sugar levels.
Antidepressants: Some antidepressants may affect glucose metabolism.
Diuretics: Certain diuretics can influence blood sugar levels.
5. Health Conditions
Insulin Resistance: Conditions like metabolic syndrome and polycystic ovary syndrome (PCOS) can lead to insulin resistance and elevated fasting glucose levels.
Thyroid Disorders: Thyroid imbalances can impact glucose metabolism and fasting glucose levels.
6. Genetics
Genetics can play a role in an individual’s susceptibility to diabetes and variations in fasting glucose levels. Family history of diabetes or metabolic disorders may influence glucose regulation.
Testing Methods for Fasting Glucose
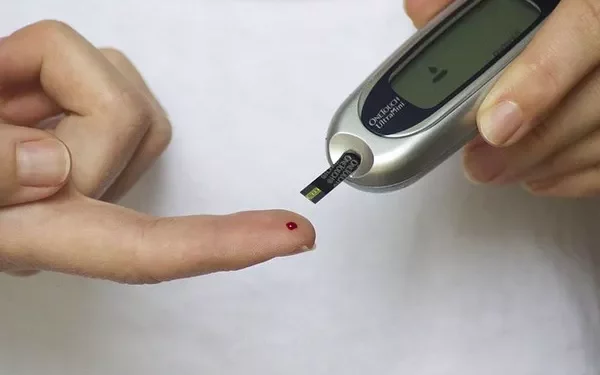
1. Blood Glucose Meter
A blood glucose meter is a portable device used to measure blood sugar levels. For fasting glucose testing, a small blood sample is typically obtained from a fingertip.
2. Laboratory Testing
Venipuncture: A blood sample is drawn from a vein and sent to a laboratory for analysis. This method provides a more accurate measurement compared to home testing.
Hematology Testing: The Hemoglobin A1c (HbA1c) test measures average blood glucose levels over the past 2-3 months. Although not a fasting test, it provides valuable information about long-term glucose control.
3. Continuous Glucose Monitoring (CGM)
CGM systems use sensors placed under the skin to continuously measure glucose levels in the interstitial fluid. While primarily used for ongoing monitoring, CGM can also provide insights into fasting glucose trends.
Managing and Improving Fasting Glucose Levels
1. Dietary Modifications
Balanced Diet: Focus on a balanced diet with whole grains, lean proteins, healthy fats, and fiber-rich fruits and vegetables.
Low Glycemic Foods: Incorporate foods with a low glycemic index to help stabilize blood sugar levels.
Portion Control: Manage portion sizes to prevent excessive carbohydrate intake.
2. Regular Physical Activity
Exercise: Engage in regular physical activity, such as walking, cycling, or strength training. Aim for at least 150 minutes of moderate-intensity exercise per week.
Consistency: Maintain a consistent exercise routine to help regulate blood glucose levels.
3. Stress Management
Relaxation Techniques: Practice stress-reducing techniques such as mindfulness, yoga, or deep breathing exercises.
Healthy Lifestyle: Ensure adequate sleep and balance work and personal life to reduce stress levels.
4. Medication Adherence
Follow Prescriptions: Adhere to prescribed medications and consult with healthcare providers if there are concerns about side effects or interactions.
Regular Monitoring: Monitor blood glucose levels as advised by healthcare professionals to assess medication effectiveness.
5. Regular Health Check-ups
Routine Testing: Schedule regular check-ups with a healthcare provider to monitor fasting glucose levels and overall health.
Early Intervention: Address any abnormal glucose levels promptly to prevent complications.
Implications of Abnormal Fasting Glucose Levels
1. Risk of Diabetes
Abnormal fasting glucose levels can indicate an increased risk of diabetes or prediabetes. Early intervention and lifestyle modifications can help manage and potentially reverse prediabetes.
2. Cardiovascular Health
Elevated fasting glucose levels are associated with an increased risk of cardiovascular diseases, including heart disease and stroke. Managing glucose levels is crucial for reducing cardiovascular risk.
3. Kidney Health
Chronic high blood glucose levels can damage the kidneys, leading to diabetic nephropathy. Regular monitoring and glucose management are essential to protect kidney function.
4. Neuropathy
Long-term elevated glucose levels can cause nerve damage, leading to diabetic neuropathy. Proper glucose control can help prevent or manage nerve-related complications.
Case Studies and Examples
Case Study 1: Type 2 Diabetes Management
A 54-year-old patient with type 2 diabetes had fasting glucose levels consistently above 120 mg/dL. With dietary modifications, regular exercise, and adherence to medication, the patient achieved fasting glucose levels within the normal range.
Case Study 2: Prediabetes Intervention
A 45-year-old individual diagnosed with prediabetes had fasting glucose levels of 110 mg/dL. Through lifestyle changes, including weight loss and increased physical activity, the patient was able to reduce fasting glucose levels and prevent the onset of diabetes.
See also: How is Blood Sugar Measured in Blood Tests?
Conclusion
Maintaining normal fasting glucose levels is essential for overall health and effective diabetes management. Understanding what constitutes a normal fasting glucose level, the factors that influence it, and the methods for testing can help individuals make informed decisions about their health. Regular monitoring, lifestyle modifications, and adherence to medical advice are crucial for achieving and maintaining optimal fasting glucose levels.
For individuals with concerns about their fasting glucose levels, consulting with a healthcare provider is essential. Personalized advice and a comprehensive management plan can help ensure effective control of blood glucose levels and prevent complications. By staying informed and proactive, individuals can successfully manage their health and reduce the risk of diabetes-related issues.
Related topics:
What Is Coding in Blood Glucose Meters?