Blood sugar monitoring is a critical aspect of diabetes management, providing valuable insights into how well an individual’s condition is controlled. One of the key times to monitor blood glucose levels is in the morning, as fasting blood sugar readings can reflect overnight glucose metabolism and overall glycemic control. This article explores what constitutes a normal blood sugar level upon waking, factors affecting morning glucose levels, and strategies for managing and interpreting these readings.
Understanding Fasting Blood Sugar Levels
Fasting blood sugar levels are measured after an overnight fast of at least eight hours, typically taken in the morning before eating or drinking anything other than water. This measurement provides a snapshot of how effectively the body manages glucose in the absence of food intake.
Normal Range for Fasting Blood Sugar
For individuals without diabetes, normal fasting blood sugar levels generally range between 70 and 99 mg/dL (3.9 to 5.5 mmol/L). This range is considered healthy and indicates proper insulin function and glucose regulation.
In individuals with diabetes, the target fasting blood sugar level can vary based on personalized treatment goals and recommendations from healthcare providers. However, a common target range for those managing diabetes is typically between 80 and 130 mg/dL (4.4 to 7.2 mmol/L). This range helps to minimize the risk of both hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar) while aiming to prevent long-term complications associated with poorly controlled diabetes.
Diagnostic Criteria for Diabetes
Fasting blood sugar levels are also used to diagnose diabetes and prediabetes. The American Diabetes Association (ADA) provides the following diagnostic criteria:
Normal: Fasting blood sugar level less than 100 mg/dL (5.6 mmol/L).
Prediabetes: Fasting blood sugar level between 100 and 125 mg/dL (5.6 to 6.9 mmol/L).
Diabetes: Fasting blood sugar level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions.
These benchmarks help categorize blood sugar levels and guide appropriate interventions and lifestyle changes.
Factors Affecting Morning Blood Sugar Levels
Several factors can influence fasting blood sugar levels upon waking. Understanding these factors is crucial for accurate interpretation and effective management of diabetes.
Insulin Sensitivity and Resistance
Insulin sensitivity refers to how effectively the body’s cells respond to insulin, a hormone that facilitates glucose uptake from the bloodstream. Insulin resistance occurs when cells become less responsive to insulin, leading to elevated blood glucose levels. This resistance can result in higher fasting blood sugar levels and is commonly seen in Type 2 diabetes.
Glycemic Variability
Glycemic variability refers to fluctuations in blood glucose levels throughout the day. Overnight glucose metabolism, including the release of glucose from the liver, can affect fasting blood sugar levels. High glycemic variability may lead to elevated morning blood sugar levels.
Dawn Phenomenon
The dawn phenomenon, also known as dawn effect, is a physiological occurrence where blood glucose levels rise in the early morning hours due to hormonal changes. Hormones such as cortisol, glucagon, and epinephrine increase insulin resistance and promote glucose production by the liver, leading to elevated fasting blood sugar levels. This phenomenon typically occurs between 2:00 AM and 8:00 AM and can be particularly pronounced in individuals with diabetes.
Medication and Insulin Regimens
Medications and insulin regimens can influence fasting blood glucose levels. For instance, certain diabetes medications, such as metformin and SGLT2 inhibitors, can help lower fasting blood sugar levels. On the other hand, medication adjustments or missed doses may lead to elevated morning glucose levels.
Diet and Evening Meals
The type and timing of evening meals can impact morning blood sugar levels. Consuming high-carbohydrate or high-fat meals close to bedtime can lead to increased glucose production overnight. Additionally, late-night snacking or irregular eating patterns may affect fasting blood glucose levels.
Sleep Patterns and Stress
Sleep quality and duration can impact blood glucose levels. Poor sleep, sleep disorders, or irregular sleep patterns can contribute to insulin resistance and elevated fasting blood sugar levels. Similarly, stress and emotional factors can influence glucose metabolism and affect morning blood sugar readings.
Physical Activity
Physical activity plays a significant role in glucose management. Regular exercise improves insulin sensitivity and helps regulate blood sugar levels. Conversely, prolonged inactivity or sedentary behavior can negatively impact glucose control and contribute to elevated fasting blood sugar levels.
Monitoring and Managing Morning Blood Sugar Levels
Effective blood sugar management requires a comprehensive approach that includes monitoring, lifestyle adjustments, and medication management. Here are strategies for managing and interpreting fasting blood glucose levels:
Regular Monitoring
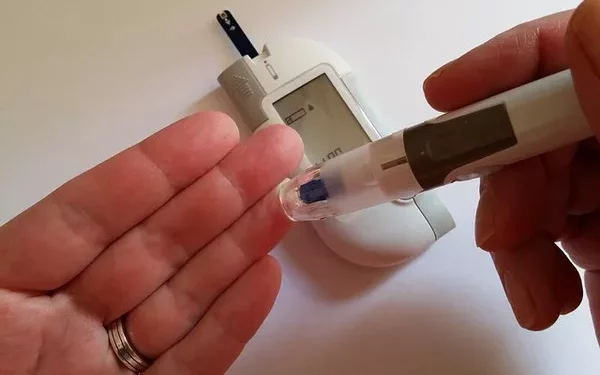
Regular monitoring of fasting blood glucose levels provides valuable data for diabetes management. Individuals should measure their blood sugar levels at the same time each morning, using a reliable glucose meter. Consistent monitoring helps identify patterns, assess the effectiveness of treatment, and make necessary adjustments.
Setting Goals
Establishing personalized blood sugar goals, in consultation with a healthcare provider, is essential for effective diabetes management. Target ranges for fasting blood sugar levels may vary based on individual health conditions, treatment plans, and lifestyle factors. Setting realistic goals helps guide daily decisions and track progress over time.
Addressing the Dawn Phenomenon
To manage the dawn phenomenon, individuals can adopt strategies such as:
Adjusting Medication: Consult with a healthcare provider about possible adjustments to medication or insulin regimens to address morning glucose spikes.
Evening Routine: Consider having a small, balanced snack before bedtime that includes protein and healthy fats to help stabilize overnight blood sugar levels.
Consistent Monitoring: Regularly monitor blood glucose levels in the early morning to identify patterns and adjust treatment as needed.
Lifestyle Modifications
Implementing lifestyle modifications can positively impact fasting blood sugar levels:
Balanced Diet: Follow a balanced diet with controlled carbohydrate intake and a focus on whole foods, including vegetables, lean proteins, and whole grains. Avoid high-carbohydrate or high-fat meals close to bedtime.
Regular Exercise: Engage in regular physical activity to improve insulin sensitivity and glucose regulation. Aim for at least 150 minutes of moderate-intensity exercise per week.
Sleep Hygiene: Prioritize good sleep hygiene by maintaining a regular sleep schedule, creating a restful sleep environment, and addressing sleep disorders if necessary.
Stress Management: Practice stress management techniques such as mindfulness, meditation, or relaxation exercises to reduce the impact of stress on blood sugar levels.
Working with Healthcare Professionals
Collaborate with healthcare professionals, including endocrinologists, dietitians, and diabetes educators, to develop a personalized diabetes management plan. These experts can provide guidance on medication adjustments, dietary recommendations, and lifestyle modifications to achieve optimal blood glucose control.
See also: What Should Blood Sugar Be When You Wake Up?
Conclusion
Normal fasting blood sugar levels upon waking are crucial for effective diabetes management and overall health. For individuals without diabetes, a normal fasting blood sugar level ranges from 70 to 99 mg/dL (3.9 to 5.5 mmol/L). For those managing diabetes, the target range is typically between 80 and 130 mg/dL (4.4 to 7.2 mmol/L), though individual goals may vary. Understanding the factors affecting morning blood glucose levels, including insulin sensitivity, glycemic variability, the dawn phenomenon, and lifestyle factors, is essential for accurate interpretation and effective management.
By implementing regular monitoring, setting personalized goals, addressing the dawn phenomenon, and making lifestyle modifications, individuals with diabetes can better manage their fasting blood sugar levels. Collaboration with healthcare professionals further supports personalized and effective diabetes management, ultimately contributing to improved glycemic control and overall well-being.
Related topics:
How Is Blood Sugar Measured in a Blood Test?