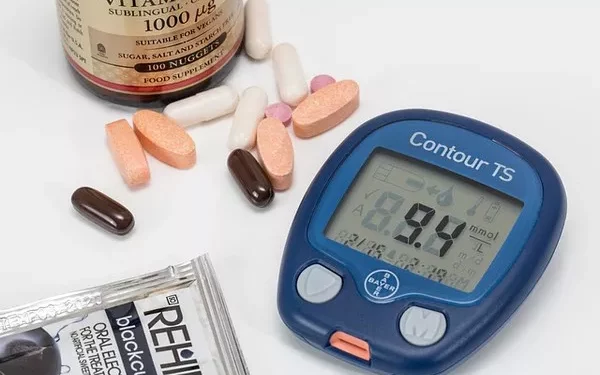
Blood sugar, or blood glucose, is a crucial measure of health, particularly for individuals with diabetes. Proper management of blood sugar levels is essential for preventing the short-term and long-term complications associated with diabetes. One of the critical aspects of blood sugar management is understanding the minimum range of blood sugar—the lowest level that is considered safe. This article will explore the minimum range of blood sugar, its significance, the risks associated with low blood sugar (hypoglycemia), and strategies to maintain blood glucose within a safe and healthy range.
Understanding Blood Sugar Levels
Blood sugar levels refer to the concentration of glucose in the blood. Glucose is the primary source of energy for the body’s cells and is derived from the carbohydrates in the food we eat. The regulation of blood sugar levels is a complex process involving the hormone insulin, which facilitates the uptake of glucose into cells, and glucagon, which signals the liver to release stored glucose when blood sugar levels are low.
For individuals without diabetes, blood sugar levels are typically maintained within a narrow range through the body’s natural regulatory mechanisms. However, for people with diabetes, these mechanisms are impaired, leading to fluctuations in blood sugar levels that can be harmful if not managed properly.
The Normal Range of Blood Sugar
Before discussing the minimum range of blood sugar, it’s important to understand what is considered a normal range. For most people, the normal fasting blood sugar range (after not eating for at least 8 hours) is between 70 and 99 milligrams per deciliter (mg/dL). After eating (postprandial), blood sugar levels typically rise and should return to less than 140 mg/dL within two hours.
For individuals with diabetes, the target blood sugar range may vary depending on the type of diabetes, the individual’s age, overall health, and the treatment plan. Generally, the American Diabetes Association (ADA) recommends the following target blood sugar ranges for adults with diabetes:
Fasting (before meals): 80-130 mg/dL
Two hours after meals: Less than 180 mg/dL
These targets may be adjusted based on individual circumstances, but they provide a general guideline for managing blood sugar levels.
What is the Minimum Safe Range of Blood Sugar?
The minimum safe range of blood sugar refers to the lowest level at which the body can function without experiencing symptoms of hypoglycemia. Hypoglycemia occurs when blood sugar levels drop below the normal range, typically below 70 mg/dL. However, the exact threshold for hypoglycemia can vary depending on the individual, their overall health, and how well their body is accustomed to low blood sugar levels.
In general, a blood sugar level below 70 mg/dL is considered low and may require intervention to prevent symptoms of hypoglycemia. However, the severity of hypoglycemia and the associated symptoms can vary depending on how low the blood sugar drops:
Mild Hypoglycemia: Blood sugar levels between 55 and 70 mg/dL may cause mild symptoms, such as shakiness, sweating, hunger, and irritability. These symptoms can usually be managed by consuming a small amount of fast-acting carbohydrates, such as glucose tablets or juice.
Moderate Hypoglycemia: Blood sugar levels between 40 and 55 mg/dL can cause more pronounced symptoms, including confusion, difficulty concentrating, dizziness, and weakness. At this stage, prompt treatment is necessary to prevent further decline in blood sugar levels.
Severe Hypoglycemia: Blood sugar levels below 40 mg/dL are considered severe and can lead to serious complications, such as seizures, loss of consciousness, and even coma. Severe hypoglycemia is a medical emergency and requires immediate treatment.
Causes of Low Blood Sugar
Several factors can contribute to low blood sugar levels, particularly for individuals with diabetes who are taking insulin or other medications to manage their condition. Understanding these causes can help individuals prevent hypoglycemia and maintain their blood sugar within a safe range.
Medications
For individuals with diabetes, certain medications, particularly insulin and sulfonylureas, can lower blood sugar levels. These medications work by increasing the amount of insulin in the body or enhancing the body’s response to insulin, which can sometimes lead to hypoglycemia if not carefully monitored.
Skipping Meals
Skipping meals or eating less than usual can result in low blood sugar levels, especially for individuals who take insulin or other diabetes medications. Without enough carbohydrates to provide glucose, blood sugar levels can drop, leading to hypoglycemia.
Increased Physical Activity
Physical activity increases the body’s demand for glucose, as muscles use glucose for energy during exercise. For individuals with diabetes, engaging in physical activity without adjusting medication or food intake can result in low blood sugar levels.
Alcohol Consumption
Alcohol can interfere with the liver’s ability to release stored glucose into the bloodstream, which can lead to low blood sugar levels. This effect is particularly pronounced when alcohol is consumed on an empty stomach or in large quantities.
Illness or Infection
Certain illnesses, such as gastrointestinal infections, can cause a decrease in appetite or an increase in the body’s use of glucose, both of which can lead to low blood sugar levels. Additionally, some infections can cause the body to produce more insulin, further lowering blood sugar levels.
Overdose of Diabetes Medications
Taking too much insulin or other diabetes medications can lead to an excessive drop in blood sugar levels. This is a common cause of hypoglycemia in individuals with diabetes and underscores the importance of carefully monitoring medication doses.
Symptoms of Low Blood Sugar
Recognizing the symptoms of low blood sugar is crucial for preventing severe hypoglycemia and its associated complications. The symptoms of low blood sugar can vary depending on the severity of the condition and the individual’s sensitivity to low blood sugar levels.
Early Symptoms
The early symptoms of low blood sugar are often related to the body’s response to a lack of glucose in the bloodstream. These symptoms include:
- Shakiness or trembling
- Sweating
- Hunger
- Irritability or mood changes
- Anxiety or nervousness
- Palpitations or rapid heartbeat
Moderate Symptoms
As blood sugar levels continue to drop, the brain begins to be affected by the lack of glucose. This can lead to more severe symptoms, such as:
- Confusion or difficulty concentrating
- Dizziness or lightheadedness
- Headache
- Weakness or fatigue
- Blurred vision
- Difficulty speaking or slurred speech
Severe Symptoms
If blood sugar levels drop to dangerously low levels, the symptoms can become life-threatening. Severe hypoglycemia can cause:
- Seizures
- Loss of consciousness
- Coma
- Death (if not treated promptly)
Treatment of Low Blood Sugar
Treating low blood sugar promptly is essential to prevent complications and restore blood sugar levels to a safe range. The specific treatment for hypoglycemia will depend on the severity of the condition and the individual’s circumstances.
Mild to Moderate Hypoglycemia
For mild to moderate hypoglycemia, the “15-15 rule” is often recommended. This involves consuming 15 grams of fast-acting carbohydrates, such as glucose tablets, juice, or regular soda, and then waiting 15 minutes before rechecking blood sugar levels. If blood sugar levels remain below 70 mg/dL, another 15 grams of carbohydrates should be consumed, and the process should be repeated until blood sugar levels return to a safe range.
Severe Hypoglycemia
Severe hypoglycemia requires immediate treatment, often involving the administration of glucagon, a hormone that raises blood sugar levels by signaling the liver to release stored glucose. Glucagon can be administered as an injection or nasal spray and is typically used when the individual is unable to eat or drink due to severe symptoms. Emergency medical assistance should be sought if severe hypoglycemia occurs.
Preventing Low Blood Sugar
Preventing low blood sugar is a critical aspect of diabetes management. By understanding the factors that contribute to hypoglycemia and taking proactive steps to avoid them, individuals with diabetes can maintain their blood sugar within a safe range and reduce the risk of complications.
Monitor Blood Sugar Levels Regularly
Regular blood sugar monitoring is essential for identifying patterns and detecting low blood sugar levels before they become severe. Individuals with diabetes should check their blood sugar levels as recommended by their healthcare provider, particularly before meals, before and after exercise, and before bedtime.
Follow a Balanced Diet
Eating regular, balanced meals that include a combination of carbohydrates, protein, and healthy fats can help maintain stable blood sugar levels. It’s important to avoid skipping meals and to eat snacks as needed to prevent blood sugar from dropping too low.
Adjust Medications as Needed
Working closely with a healthcare provider to adjust insulin or other diabetes medications based on blood sugar levels, diet, and physical activity is crucial for preventing hypoglycemia. Individuals should never adjust their medication doses without consulting their healthcare provider.
Be Prepared for Hypoglycemia
Individuals with diabetes should always carry a source of fast-acting carbohydrates, such as glucose tablets or candy, to treat low blood sugar quickly if it occurs. Additionally, wearing a medical alert bracelet or carrying a diabetes identification card can help others provide appropriate assistance in case of severe hypoglycemia.
Limit Alcohol Consumption
Alcohol can interfere with blood sugar regulation, so it’s important for individuals with diabetes to limit their alcohol consumption and to eat when drinking to prevent hypoglycemia. Drinking in moderation and avoiding excessive alcohol intake can help maintain stable blood sugar levels.
The Importance of Education and Support
Understanding the minimum range of blood sugar and the risks associated with low blood sugar is essential for individuals with diabetes and their caregivers. Education and support from healthcare providers, diabetes educators, and support groups can empower individuals to manage their condition effectively and prevent hypoglycemia.
Healthcare providers play a crucial role in educating patients about the signs and symptoms of low blood sugar, the importance of regular monitoring, and the strategies for preventing and treating hypoglycemia. Patients should feel comfortable discussing their concerns and asking questions about their diabetes management plan.
See also: Is There a Way to Check Blood Sugar Without Needles?
Conclusion
The minimum range of blood sugar is a critical aspect of diabetes management, as maintaining blood sugar levels above the threshold for hypoglycemia is essential for preventing complications and ensuring overall health and well-being. By understanding the causes, symptoms, and treatment of low blood sugar, individuals with diabetes can take proactive steps to manage their condition effectively and reduce the risk of hypoglycemia. Through regular monitoring, a balanced diet, appropriate medication management, and education, individuals can maintain their blood sugar within a safe and healthy range, leading to better long-term outcomes and quality of life.
Related topics:
Is There a Way to Constantly Monitor Blood Sugar?