Monitoring blood sugar levels is a critical aspect of managing diabetes, and understanding what your blood sugar should be when you wake up is particularly important. Fasting blood glucose levels, or those measured after an overnight fast, provide crucial information about your body’s ability to regulate blood sugar and can help guide diabetes management strategies. This article delves into the optimal range for blood sugar levels upon waking, factors affecting these levels, and how to manage and interpret them effectively.
Understanding Fasting Blood Glucose Levels
Fasting blood glucose is measured after an overnight fast of at least 8-12 hours, typically in the morning before eating breakfast. This measurement is used to assess how well your body is managing blood sugar levels when it is not influenced by recent food intake. It provides a snapshot of your basal glucose control and is a key indicator of overall diabetes management.
Optimal Fasting Blood Glucose Levels:
Normal Range: For individuals without diabetes, a fasting blood glucose level is typically between 70 and 99 mg/dL (3.9 to 5.5 mmol/L).
Prediabetes: Fasting blood glucose levels ranging from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) may indicate prediabetes, a condition where blood sugar levels are higher than normal but not high enough for a diabetes diagnosis.
Diabetes: A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions is usually indicative of diabetes.
Factors Affecting Fasting Blood Glucose Levels
Several factors can influence fasting blood glucose levels, including diet, medication, physical activity, stress, and sleep quality. Understanding these factors can help you better manage your blood sugar levels and make necessary adjustments to your diabetes management plan.
Diet and Nutrition
The foods you eat and when you eat them can significantly impact your blood glucose levels. A diet high in carbohydrates, especially refined sugars and starches, can lead to higher fasting blood glucose levels. Conversely, a balanced diet with a focus on low-GI (glycemic index) foods, high fiber, and lean proteins can help maintain stable blood sugar levels.
Key Dietary Considerations:
Avoid Late-Night Snacks: Eating large or carbohydrate-rich meals before bedtime can elevate fasting blood glucose levels.
Balanced Evening Meals: Aim for a balanced dinner with a mix of protein, healthy fats, and low-GI carbohydrates to support stable blood sugar levels overnight.
Medication and Insulin Use
For individuals with diabetes, medication and insulin therapy play a crucial role in blood glucose management. The timing, type, and dosage of insulin or oral medications can affect fasting blood glucose levels.
Key Points:
Medication Adherence: Consistently taking your prescribed medications as directed is essential for maintaining optimal blood sugar levels.
Insulin Adjustments: Your healthcare provider may need to adjust your insulin regimen based on your fasting blood glucose levels to ensure effective control.
Physical Activity
Regular physical activity helps improve insulin sensitivity and lower blood glucose levels. Exercise can lower blood sugar levels both during and after physical activity.
Key Points:
Regular Exercise: Incorporate regular physical activity into your routine to help manage blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week.
Timing: The timing of exercise relative to your meals and medication can impact your fasting blood glucose levels.
Sleep Quality
Adequate and quality sleep is essential for overall health and blood sugar regulation. Poor sleep can lead to insulin resistance and higher fasting blood glucose levels.
Key Points:
Sleep Duration: Aim for 7-9 hours of quality sleep each night.
Sleep Disorders: Conditions such as sleep apnea can affect blood glucose control. If you suspect sleep issues, consult with a healthcare provider.
Stress and Emotional Well-being
Stress can affect blood sugar levels by increasing the release of stress hormones like cortisol, which can raise blood glucose levels.
Key Points:
Stress Management: Practice stress-reducing techniques such as mindfulness, meditation, and relaxation exercises.
Emotional Support: Seek support from healthcare providers, counselors, or support groups if needed.
Monitoring and Managing Fasting Blood Glucose Levels
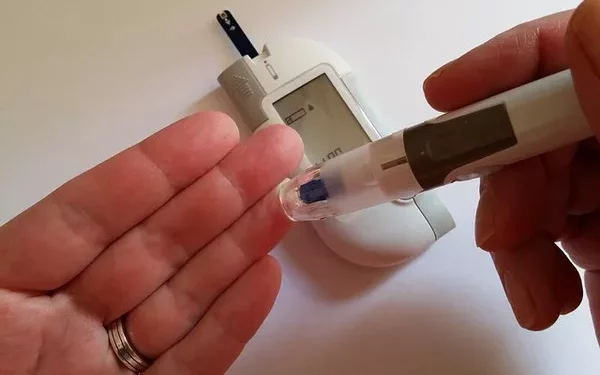
Regular monitoring of fasting blood glucose levels is essential for effective diabetes management. Here are some strategies and tips for managing and interpreting your fasting blood glucose levels:
Regular Testing
Consistent testing helps track changes in your blood sugar levels and assess the effectiveness of your diabetes management plan.
Tips:
Test at the Same Time Each Day: For consistency, test your blood glucose at the same time each morning before eating or drinking anything.
Record Results: Keep a log of your fasting blood glucose levels, along with any relevant notes about diet, medication, and activities.
Interpreting Results
Understanding what your fasting blood glucose levels indicate about your diabetes management is crucial for making necessary adjustments.
Interpretation:
Consistently High Levels: If your fasting blood glucose levels are consistently above the target range, consult with your healthcare provider to review your treatment plan and make adjustments as needed.
Normal or Low Levels: Consistently within the target range indicates good blood sugar control, but continue to monitor and maintain your management strategies.
Consulting with Healthcare Providers
Regular consultations with healthcare providers are important for effective diabetes management.
Key Points:
Discuss Concerns: Share any concerns or observations about your fasting blood glucose levels with your healthcare provider.
Adjustments: Your provider may recommend changes to your medication, diet, or lifestyle based on your fasting blood glucose levels.
Strategies for Achieving Optimal Fasting Blood Glucose Levels
Achieving and maintaining optimal fasting blood glucose levels involves a combination of dietary adjustments, lifestyle changes, and medical management. Here are some strategies to help you reach your goals:
Dietary Adjustments
Carbohydrate Counting: Keep track of carbohydrate intake to avoid spikes in blood glucose levels.
Portion Control: Monitor portion sizes to manage calorie intake and prevent overeating.
Healthy Eating: Focus on whole foods, including vegetables, fruits, lean proteins, and whole grains.
Lifestyle Changes
Regular Exercise: Incorporate physical activity into your daily routine to improve insulin sensitivity and lower blood glucose levels.
Stress Management: Engage in stress-reducing activities and seek support if needed.
Adequate Sleep: Prioritize quality sleep to support overall health and blood sugar regulation.
Medical Management
Medication Adherence: Follow your prescribed medication regimen and discuss any concerns with your healthcare provider.
Regular Monitoring: Monitor your blood glucose levels regularly to track changes and adjust your management plan as needed.
See also: Is There a Fitbit That Tracks Blood Sugar?
Conclusion
Understanding what your blood sugar should be when you wake up is crucial for effective diabetes management. Optimal fasting blood glucose levels typically range from 70 to 99 mg/dL (3.9 to 5.5 mmol/L) for individuals without diabetes. For those with diabetes, achieving fasting blood glucose levels within target ranges requires a combination of dietary adjustments, lifestyle changes, and consistent medical management.
Regular monitoring, adherence to treatment plans, and consultations with healthcare providers are key to maintaining optimal fasting blood glucose levels and overall health. By adopting a comprehensive approach to managing your blood sugar, you can achieve better control and improve your quality of life.
Related topics:
How Often Are Blood Sugars Checked in Hospital?