Hyperglycemia, or high blood glucose, is a condition frequently associated with diabetes mellitus. It is characterized by blood sugar levels that exceed the normal range. Managing hyperglycemia is crucial for preventing both short-term complications and long-term damage associated with diabetes. One common question that arises is whether it is safe or advisable to consume sugar when experiencing hyperglycemia. This article will delve into the intricacies of hyperglycemia, the role of dietary sugar, and provide guidance for managing blood glucose levels effectively.
Understanding Hyperglycemia
Hyperglycemia occurs when there is too much glucose in the blood. This can happen for a variety of reasons, including insufficient insulin production, insulin resistance, excessive carbohydrate intake, stress, illness, and certain medications. The normal fasting blood glucose level is typically between 70 and 100 mg/dL. Hyperglycemia is generally defined as a blood glucose level exceeding 125 mg/dL when fasting or over 180 mg/dL two hours after eating.
Symptoms and Risks of Hyperglycemia
Symptoms of hyperglycemia may include increased thirst, frequent urination, fatigue, blurred vision, and headaches. If left untreated, chronic hyperglycemia can lead to serious complications such as neuropathy, retinopathy, nephropathy, cardiovascular disease, and can even result in diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), both of which are medical emergencies.
The Role of Sugar in the Diet
Sugar, in its various forms, is a carbohydrate. Carbohydrates are one of the three macronutrients essential for human life, providing a primary source of energy. However, not all carbohydrates are created equal. Simple sugars, like glucose, fructose, and sucrose, are rapidly absorbed into the bloodstream, leading to quick spikes in blood glucose levels. Complex carbohydrates, such as those found in whole grains, legumes, and vegetables, are broken down more slowly, providing a more gradual release of glucose into the bloodstream.
The Impact of Sugar on Blood Glucose Levels
When someone with diabetes consumes sugar, it can cause a rapid increase in blood glucose levels. This is particularly problematic for individuals who have hyperglycemia, as their blood glucose levels are already elevated. Consuming additional sugar in this state can exacerbate hyperglycemia and lead to further complications.
Can You Eat Sugar with Hyperglycemia?
Given the rapid impact of sugar on blood glucose levels, it is generally advisable to avoid consuming sugar when experiencing hyperglycemia. Instead, the focus should be on stabilizing and lowering blood glucose levels through other means. Here are some key considerations and strategies for managing hyperglycemia without the consumption of sugar:
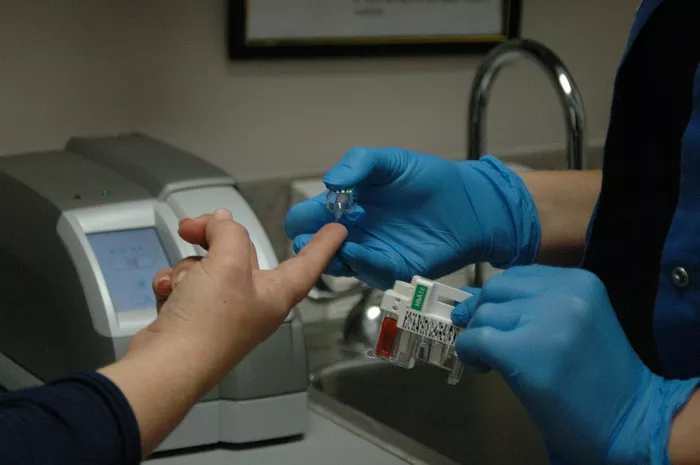
Monitoring Blood Glucose Levels
Frequent monitoring of blood glucose levels is crucial for individuals with diabetes. This allows for timely adjustments in diet, medication, and lifestyle to maintain blood glucose within the target range. Using a continuous glucose monitor (CGM) or regular blood glucose tests can help track how different foods and activities affect blood glucose levels.
Dietary Modifications
- Carbohydrate Counting: Understanding the carbohydrate content of foods and managing portions can help prevent spikes in blood glucose levels. Emphasizing complex carbohydrates over simple sugars is beneficial.
- Low Glycemic Index Foods: Foods with a low glycemic index (GI) release glucose more slowly into the bloodstream, helping to maintain stable blood glucose levels. Examples include whole grains, legumes, non-starchy vegetables, and most fruits.
- Balanced Meals: Incorporating a balance of carbohydrates, proteins, and fats in each meal can slow the absorption of glucose and prevent rapid spikes in blood glucose levels. Proteins and fats do not raise blood glucose levels significantly and can help provide sustained energy.
- Fiber-Rich Foods: Dietary fiber, particularly soluble fiber, can help slow the absorption of glucose and improve blood sugar control. High-fiber foods include vegetables, fruits, legumes, and whole grains.
Physical Activity
Regular physical activity can help lower blood glucose levels and improve insulin sensitivity. Aerobic exercises like walking, cycling, and swimming, as well as resistance training, are beneficial. It’s important to monitor blood glucose levels before and after exercise to understand its impact and adjust accordingly.
Medication Management
For individuals on insulin or other diabetes medications, proper management is essential. This may include adjusting doses based on blood glucose readings, meals, and physical activity. Consulting with a healthcare provider to tailor medication regimens to individual needs is important.
Stress Management
Stress can cause blood glucose levels to rise due to the release of stress hormones like cortisol. Techniques such as mindfulness, meditation, yoga, and deep-breathing exercises can help manage stress and, in turn, aid in maintaining stable blood glucose levels.
Hydration
Staying well-hydrated is important, as high blood glucose levels can lead to dehydration. Drinking water can help flush out excess glucose through urine and keep the body functioning optimally.
Special Considerations
Hypoglycemia Risk
While managing hyperglycemia, it’s important to be aware of the risk of hypoglycemia, or low blood glucose. This can occur if blood glucose levels drop too rapidly or too low. Symptoms of hypoglycemia include shakiness, sweating, confusion, and dizziness. In such cases, consuming a small amount of fast-acting carbohydrate, such as glucose tablets or juice, is necessary to raise blood glucose levels promptly.
Individualized Care
Diabetes management is highly individualized. What works for one person may not work for another. Factors such as age, type of diabetes, overall health, lifestyle, and personal preferences all play a role in determining the best approach to managing hyperglycemia. Regular consultations with healthcare providers, including endocrinologists, dietitians, and diabetes educators, are essential for personalized care.
Special Populations
Certain populations, such as pregnant women with gestational diabetes, children with type 1 diabetes, and older adults, may require special considerations for managing hyperglycemia. Pregnancy requires tight glucose control to ensure the health of both mother and baby. Children and adolescents need tailored management plans that accommodate their growth and activity levels. Older adults may have other health conditions or medications that impact blood glucose management.
Conclusion
In conclusion, while the immediate consumption of sugar is not advisable when experiencing hyperglycemia, managing blood glucose levels involves a multifaceted approach that includes careful dietary planning, regular physical activity, appropriate medication use, and stress management. By focusing on a balanced diet that emphasizes complex carbohydrates, low glycemic index foods, and adequate fiber, individuals with diabetes can better control their blood glucose levels and prevent the complications associated with hyperglycemia.
Regular monitoring and personalized care plans are essential for effective diabetes management. Each individual’s needs may vary, and it is crucial to work closely with healthcare providers to develop a strategy that works best for them. By adopting a comprehensive approach to diabetes management, individuals can maintain better control over their blood glucose levels and lead healthier, more active lives.
Related topics:
Can Hyperglycemia Cause High Blood Pressure?