Diabetes is a chronic condition characterized by high levels of glucose (sugar) in the blood. Managing diabetes effectively involves understanding various factors that influence blood sugar levels, one of which is the A1C test. In this article, we will explore what A1C is, its significance in diabetes management, and how it can help individuals maintain better control over their condition.
What is A1C?
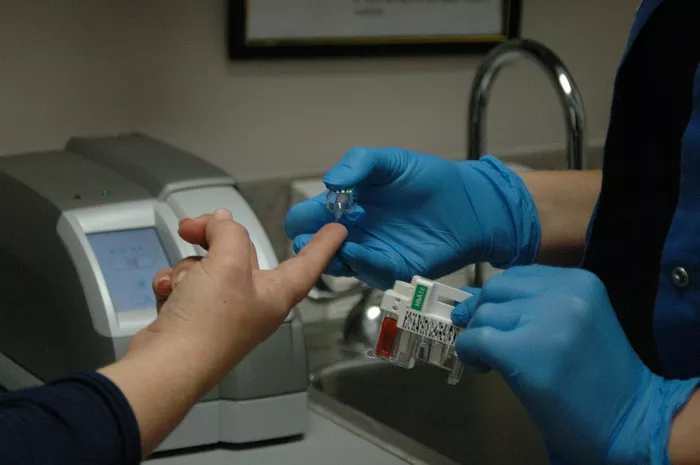
A1C, also known as glycated hemoglobin, is a blood test that measures the average blood sugar levels over the past two to three months. Unlike daily blood sugar tests, which provide a snapshot of glucose levels at a specific moment, the A1C test reflects a broader picture of blood sugar control over time. This makes it a valuable tool for assessing long-term diabetes management.
Normal A1C Range
For individuals without diabetes, the typical A1C range falls between 4% and 5.6%. This range indicates healthy blood sugar levels and minimal risk of developing diabetes-related complications. However, it’s essential to note that individual factors, such as age and underlying health conditions, can influence A1C levels.
Diabetes Diagnosis and A1C
A1C levels play a crucial role in diagnosing diabetes. According to established medical guidelines, a diagnosis of diabetes is typically made when A1C levels reach 6.5% or higher. This threshold indicates significant impairment in blood sugar control and confirms the presence of diabetes.
A1C Levels and Diabetes
Once diagnosed with diabetes, individuals must understand how A1C levels correlate with their condition. A1C levels equal to or greater than 6.5% suggest poor blood sugar control and an increased risk of diabetes-related complications, such as cardiovascular disease, kidney damage, and nerve damage.
Interpretation of Results
If someone’s A1C level falls within the range indicating diabetes, it’s crucial to interpret the results accurately. A higher A1C level signifies a greater risk of diabetes-related complications and the need for more aggressive management strategies. It’s essential to consult with a healthcare professional to develop a personalized treatment plan tailored to individual needs.
Monitoring and Management
Monitoring A1C levels over time is essential for tracking diabetes management progress and adjusting treatment accordingly. Regular A1C testing allows healthcare providers to assess the effectiveness of current treatment regimens and make informed decisions about medication adjustments or lifestyle modifications.
Prevention and Control
While diabetes is a chronic condition, there are steps individuals can take to prevent or manage it effectively. Adopting a healthy lifestyle that includes regular exercise, a balanced diet, and maintaining a healthy weight can reduce the risk of developing type 2 diabetes. For those already diagnosed, proper diabetes management, including regular monitoring of A1C levels, medication adherence, and lifestyle modifications, can help prevent complications and improve overall quality of life.
Conclusion
Understanding A1C and its role in diabetes management is essential for individuals living with diabetes. By regularly monitoring A1C levels, making lifestyle modifications, and working closely with healthcare providers, individuals can take control of their condition and reduce the risk of diabetes-related complications. A comprehensive approach to diabetes management, focusing on both medical and lifestyle factors, is key to achieving optimal health outcomes and improving overall well-being.
Related Topics:
What is the Difference Between Glucose Test & HbA1c?
Plasma Glucose vs Blood Glucose: What is the Difference?
Do Any Smart Watches Measure Blood Sugar?