Herpes simplex virus type 1 (HSV-1) is a prevalent viral infection affecting millions worldwide. While HSV-1 primarily manifests as oral herpes, causing cold sores or fever blisters, it can also lead to genital herpes through oral-genital contact. One of the most perplexing aspects of HSV-1 is its tendency to recur, with outbreaks causing discomfort and distress to those affected. Understanding the triggers behind HSV-1 outbreaks is crucial for managing the condition effectively and improving the quality of life for those living with herpes. In this article, we delve into the various factors that contribute to HSV-1 recurrence, shedding light on the complex interplay of biological, environmental, and lifestyle influences.
Introduction to HSV-1: A Brief Overview
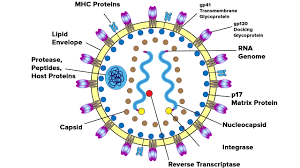
HSV-1 belongs to the Herpesviridae family and is one of the most common human viruses. It is highly contagious and spreads through direct contact with an infected individual, particularly during episodes of active viral shedding. Once contracted, the virus remains dormant in nerve cells, primarily in the trigeminal ganglion for oral herpes and the sacral ganglia for genital herpes. Periodically, the virus reactivates, leading to recurrent outbreaks characterized by the formation of painful blisters or sores on the affected area.
Biological Factors Influencing HSV-1 Recurrence
Viral Reactivation Mechanisms: The primary trigger for HSV-1 recurrence is the reactivation of the latent virus from sensory ganglia. Various factors can induce viral reactivation, including stress, hormonal changes, and compromised immune function. Reactivation involves the migration of viral particles along the sensory nerves to the skin or mucous membranes, where they cause lesions characteristic of herpes outbreaks.
Immune System Dynamics: The immune system plays a critical role in controlling HSV-1 infection and preventing recurrent outbreaks. T-cell-mediated immunity, particularly CD8+ cytotoxic T cells, is essential for suppressing viral replication and maintaining latency. However, factors such as immunosuppression due to illness, medications, or stress can weaken the immune response, facilitating viral reactivation and subsequent outbreaks.
Genetic Predisposition: Genetic factors may influence an individual’s susceptibility to HSV-1 infection and their propensity for recurrent outbreaks. Variations in genes involved in immune regulation and viral latency, such as those encoding cytokines and human leukocyte antigens (HLAs), can impact the frequency and severity of herpes recurrences.
Environmental Triggers and Lifestyle Factors
Ultraviolet (UV) Radiation: Exposure to sunlight, particularly ultraviolet (UV) radiation, has been implicated as a trigger for HSV-1 outbreaks, especially oral herpes. UV radiation can induce local immunosuppression in the skin, impairing the body’s ability to control viral reactivation. Additionally, sunlight exposure may cause physical trauma to the lips, facilitating the entry of the virus and triggering a cold sore flare-up.
Temperature and Weather Changes: Extreme temperatures and weather fluctuations, such as cold weather or sudden changes from hot to cold environments, can precipitate HSV-1 outbreaks. Cold temperatures may compromise local immune responses, while dry air can lead to dehydration of the skin and mucous membranes, creating favorable conditions for viral reactivation.
Trauma or Injury: Physical trauma or injury to the affected area can serve as a trigger for HSV-1 recurrence. Minor abrasions or cuts on the lips or mouth can provide an entry point for the virus, leading to the development of cold sores or fever blisters. Additionally, dental procedures, lip biting, or vigorous oral activities may exacerbate existing lesions or induce new outbreaks.
Psychological Stress: Stress is a well-established trigger for HSV-1 reactivation, with emotional or psychological stressors often preceding outbreaks. Stress disrupts immune function and hormonal balance, promoting viral replication and compromising the body’s ability to suppress HSV-1 reactivation. Common stressors such as work pressure, relationship issues, or major life events can trigger recurrent herpes outbreaks in susceptible individuals.
Hormonal Fluctuations: Hormonal changes, particularly fluctuations in estrogen and progesterone levels, can influence HSV-1 recurrence, especially in women. Hormonal shifts occurring during menstruation, pregnancy, or menopause may disrupt the delicate balance between viral latency and reactivation, increasing the likelihood of outbreaks. Oral contraceptives or hormone replacement therapy (HRT) may also impact the frequency and severity of herpes recurrences in some individuals.
Nutritional Factors: Diet and nutritional status can influence immune function and susceptibility to HSV-1 outbreaks. Deficiencies in certain vitamins and minerals, such as vitamin D, vitamin C, zinc, and lysine, have been associated with increased herpes recurrence rates. Conversely, a balanced diet rich in immune-supportive nutrients and lysine-containing foods may help reduce the frequency and severity of outbreaks in individuals with HSV-1.
Behavioral and Preventive Strategies
Stress Management Techniques: Adopting stress-reduction strategies such as mindfulness meditation, deep breathing exercises, yoga, or cognitive-behavioral therapy (CBT) can help mitigate the impact of psychological stress on HSV-1 recurrence. Engaging in regular physical activity, maintaining a healthy work-life balance, and seeking social support are also beneficial for managing stress and promoting overall well-being.
Sun Protection: Individuals prone to oral herpes outbreaks triggered by sunlight exposure should take preventive measures to protect their lips and face from UV radiation. This includes wearing broad-spectrum sunscreen with a high sun protection factor (SPF), using lip balms or creams containing SPF, and wearing hats or using umbrellas to provide additional shade.
Temperature Regulation: To minimize the risk of HSV-1 outbreaks associated with temperature changes, individuals should dress appropriately for the weather and avoid prolonged exposure to extreme temperatures. In cold weather, protecting the lips with scarves or avoiding direct exposure to cold winds can help prevent cold sore flare-ups.
Oral Hygiene Practices: Maintaining good oral hygiene is essential for reducing the risk of HSV-1 transmission and recurrent outbreaks. This includes practicing regular brushing and flossing, avoiding sharing utensils or personal items with others, and refraining from oral contact during active herpes lesions.
Healthy Lifestyle Choices: Adopting a healthy lifestyle characterized by balanced nutrition, adequate hydration, regular exercise, and sufficient sleep can bolster immune function and reduce the likelihood of HSV-1 recurrence. Avoiding excessive alcohol consumption, tobacco use, and illicit drug use is also important for overall health and herpes management.
Conclusion
HSV-1 outbreaks can significantly impact the physical, emotional, and social well-being of affected individuals, necessitating effective strategies for outbreak prevention and management. By understanding the various triggers and risk factors associated with HSV-1 recurrence, individuals can empower themselves to make informed lifestyle choices and adopt preventive measures to minimize the frequency and severity of outbreaks. Furthermore, ongoing research into the pathogenesis of HSV-1 and the development of novel therapeutic interventions hold promise for improving the management of this common viral infection in the future.