Insulin pumps have revolutionized diabetes management by providing a convenient and effective way for individuals with diabetes to administer insulin. These devices deliver insulin continuously, mimicking the function of a healthy pancreas. However, understanding the type of insulin used in these pumps is crucial for both healthcare professionals and patients. In this article, we delve into the various types of insulin used in insulin pumps, their mechanisms of action, and considerations for optimal management.
Introduction to Insulin Pumps
Insulin pumps are small, computerized devices that deliver rapid-acting insulin continuously throughout the day, as well as additional doses at meal times. Unlike traditional insulin injections, which require multiple daily injections and may result in variable absorption rates, insulin pumps offer precise insulin delivery tailored to individual needs.
The key components of an insulin pump include:
Insulin Reservoir: A reservoir holds the insulin within the pump.
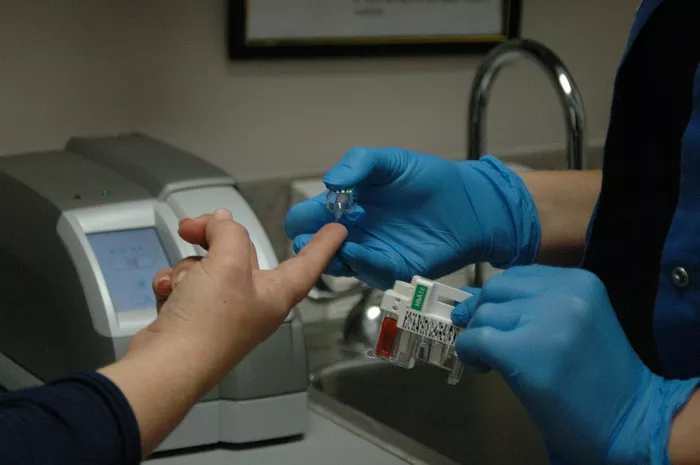
Infusion Set: This set includes a thin tube (cannula) that is inserted under the skin to deliver insulin continuously.
Insulin Pump: The pump itself houses the electronics, including a processor and a user interface for programming and monitoring.
Insulin pumps offer several advantages over traditional insulin injection regimens, including:
Improved Glycemic Control: Continuous insulin delivery can help maintain stable blood glucose levels, reducing the risk of hypo- and hyperglycemia.
Flexibility: Users can adjust basal insulin rates and administer bolus doses to match their lifestyle and activity levels.
Convenience: With fewer injections required, insulin pump therapy offers greater convenience and flexibility for managing diabetes.
Types of Insulin Used in Insulin Pumps
Insulin pumps typically use rapid-acting insulin analogs, which closely mimic the physiological insulin response after meals. These insulins are characterized by their rapid onset of action, peak concentration, and relatively short duration of action. The two main types of rapid-acting insulin analogs used in insulin pumps are:
Insulin Lispro (Humalog): Lispro insulin is a synthetic analog of human insulin that has a rapid onset of action, reaching peak levels within 30 to 90 minutes after injection. Its duration of action is approximately 3 to 5 hours, making it suitable for bolus dosing with meals.
Insulin Aspart (NovoLog/NovoRapid): Aspart insulin is another rapid-acting analog that shares similar pharmacokinetic properties with Lispro insulin. It has a rapid onset of action, with peak levels occurring within 40 to 50 minutes after injection, and a duration of action of approximately 3 to 5 hours.
These rapid-acting insulin analogs are preferred for use in insulin pumps due to their fast onset and short duration of action, which closely mimic the physiological insulin secretion in response to food intake.
Mechanism of Action of Rapid-Acting Insulin Analogs
Rapid-acting insulin analogs exert their effects by promoting glucose uptake into cells and inhibiting hepatic glucose production. Upon subcutaneous injection, these analogs are rapidly absorbed into the bloodstream, allowing for a quick onset of action.
Once in the bloodstream, rapid-acting insulin analogs bind to insulin receptors on target cells, primarily muscle, fat, and liver cells. This binding activates intracellular signaling pathways that facilitate the translocation of glucose transporter proteins (GLUT4) to the cell membrane. As a result, glucose uptake is enhanced, leading to a decrease in blood glucose levels.
Additionally, rapid-acting insulin analogs suppress the release of glucose from the liver (hepatic glucose production), further contributing to their glucose-lowering effects. By closely mimicking the physiological insulin response, these analogs help regulate blood glucose levels in individuals with diabetes.
Considerations for Insulin Pump Therapy
While insulin pumps offer numerous benefits for diabetes management, there are several considerations to keep in mind when initiating pump therapy or adjusting insulin regimens:
Basal Rate Adjustment: Basal insulin rates should be individualized based on factors such as age, weight, activity level, and metabolic requirements. Close monitoring of blood glucose levels and adjustments to basal rates may be necessary to achieve optimal glycemic control.
Bolus Calculations: Insulin pumps allow users to calculate bolus doses based on factors such as carbohydrate intake, current blood glucose levels, and insulin sensitivity. Proper education and training on carbohydrate counting and insulin dosing algorithms are essential for safe and effective pump use.
Site Rotation: Regular rotation of infusion sites is crucial to prevent the development of lipohypertrophy (thickened, fatty tissue) and ensure optimal insulin absorption. Insulin absorption may be compromised if infusion sites are not rotated regularly, leading to unpredictable blood glucose levels.
Monitoring and Maintenance: Regular monitoring of blood glucose levels, insulin pump settings, and infusion site integrity is essential for detecting and preventing complications such as hyperglycemia, hypoglycemia, and pump malfunction. Users should be educated on troubleshooting techniques and when to seek assistance from healthcare providers.
Psychosocial Factors: Psychological and social factors can impact adherence to insulin pump therapy, including fear of technology, financial concerns, and lifestyle preferences. Healthcare providers should address these factors and provide support to facilitate successful pump use.
Conclusion
Insulin pumps have revolutionized diabetes management by providing a convenient and effective way to administer insulin. Rapid-acting insulin analogs, such as insulin lispro and insulin aspart, are the preferred types of insulin used in insulin pumps due to their fast onset of action and short duration of action.
Understanding the mechanism of action of rapid-acting insulin analogs and considerations for insulin pump therapy is crucial for optimizing glycemic control and improving quality of life for individuals with diabetes. Healthcare providers play a vital role in educating patients about insulin pump therapy, monitoring treatment outcomes, and providing ongoing support to ensure safe and effective pump use. With proper education, training, and support, insulin pump therapy can empower individuals with diabetes to better manage their condition and lead healthier lives.