In the realm of chronic diseases, few conditions evoke as much fear and uncertainty as diabetes. With its far-reaching impacts on health and well-being, diabetes presents a formidable challenge for individuals, healthcare providers, and society as a whole.
While both type 1 and type 2 diabetes share the common characteristic of elevated blood sugar levels, they are distinct conditions with unique underlying mechanisms, implications, and management approaches.
In this comprehensive exploration, we delve into the complexities of type 1 diabetes and shed light on why it is often considered more challenging than type 2 diabetes.
Differentiating Between Type 1 and Type 2 Diabetes
Before delving into the nuances of type 1 diabetes, it’s essential to understand the key differences between type 1 and type 2 diabetes:
Type 1 Diabetes:
Type 1 diabetes, also known as insulin-dependent diabetes or juvenile diabetes, is an autoimmune condition in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas.
As a result, individuals with type 1 diabetes produce little to no insulin, the hormone responsible for regulating blood sugar levels. Type 1 diabetes typically develops during childhood or adolescence but can occur at any age.
Type 2 Diabetes:
Type 2 diabetes, the most common form of diabetes, is characterized by insulin resistance, where the body’s cells become less responsive to the effects of insulin.
Initially, the pancreas compensates by producing more insulin to overcome this resistance. However, over time, insulin production may decline, leading to elevated blood sugar levels.
Type 2 diabetes is closely linked to lifestyle factors such as obesity, sedentary behavior, poor dietary choices, and genetic predisposition.
The Unique Challenges of Type 1 Diabetes
While both type 1 and type 2 diabetes pose significant health risks and complications, type 1 diabetes presents several unique challenges:
1. Absolute Insulin Deficiency:
Unlike type 2 diabetes, where insulin resistance is the primary mechanism, type 1 diabetes is characterized by an absolute deficiency of insulin. Without insulin, the body cannot effectively transport glucose from the bloodstream into cells for energy production, leading to hyperglycemia (elevated blood sugar levels) and metabolic imbalances.
2. Dependence on Exogenous Insulin:
Individuals with type 1 diabetes require lifelong insulin therapy to survive. Unlike type 2 diabetes, where insulin therapy may be prescribed in later stages of the disease, type 1 diabetes necessitates immediate and continuous administration of exogenous (external) insulin to maintain blood sugar levels within target ranges.
This reliance on insulin therapy adds an additional layer of complexity to diabetes management and requires meticulous monitoring and adjustment of insulin doses to match fluctuating metabolic needs.
3. Risk of Diabetic Ketoacidosis (DKA):
Without adequate insulin, the body’s cells are unable to access glucose for energy production and may turn to alternative fuel sources, such as fat. This can lead to the production of ketones, acidic byproducts that can accumulate in the bloodstream and result in a life-threatening condition known as diabetic ketoacidosis (DKA).
DKA is more common in individuals with type 1 diabetes and requires prompt medical intervention to prevent complications such as organ failure and coma.
3. Unpredictable Blood Sugar Variability:
Managing blood sugar levels in type 1 diabetes can be inherently challenging due to the unpredictability of factors such as food intake, physical activity, stress, illness, and hormonal fluctuations. Unlike type 2 diabetes, where lifestyle modifications and oral medications may provide some degree of glycemic control, type 1 diabetes requires constant vigilance and adjustment of insulin doses to navigate fluctuations in blood sugar levels.
4. Emotional and Psychological Impact:
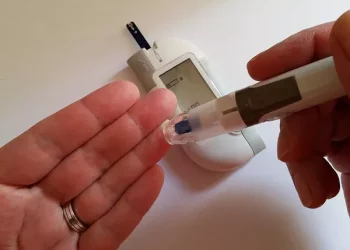
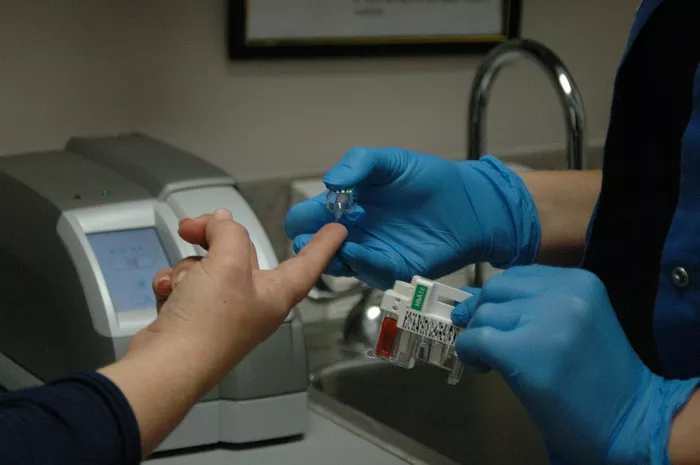
Living with type 1 diabetes can take a toll on emotional and psychological well-being, particularly for children, adolescents, and young adults. The burden of daily diabetes management tasks, such as blood sugar monitoring, insulin administration, carbohydrate counting, and meal planning, can lead to feelings of anxiety, stress, burnout, and social isolation.
Additionally, the fear of hypoglycemia (low blood sugar) and the relentless nature of diabetes management can impact quality of life and mental health outcomes.
The Importance of Diabetes Management and Support
Despite the unique challenges posed by type 1 diabetes, effective management strategies and support systems can empower individuals to live fulfilling and healthy lives:
1. Comprehensive Diabetes Education:
Providing individuals with type 1 diabetes and their families with comprehensive education and support is essential for successful diabetes management. This includes understanding the basics of diabetes, insulin therapy, blood sugar monitoring, carbohydrate counting, and recognizing and responding to hypo- and hyperglycemia.
2. Personalized Diabetes Care Plans:
Diabetes management should be tailored to the individual needs, preferences, and goals of each person with type 1 diabetes. This may involve collaborating with a multidisciplinary healthcare team, including endocrinologists, certified diabetes educators, dietitians, psychologists, and social workers, to develop personalized care plans that address physical, emotional, and psychological aspects of diabetes management.
3. Continuous Glucose Monitoring (CGM) and Insulin Pump Therapy:
Advancements in technology, such as continuous glucose monitoring (CGM) systems and insulin pump therapy, have revolutionized diabetes management by providing real-time insights into blood sugar trends and allowing for more precise insulin delivery. CGM systems can help individuals with type 1 diabetes make informed decisions about insulin dosing, diet, and lifestyle modifications to optimize glycemic control and reduce the risk of complications.
4. Peer Support and Community Engagement:
Connecting with peers, support groups, and online communities can provide valuable emotional support, encouragement, and practical tips for navigating the challenges of living with type 1 diabetes. Peer support networks offer opportunities for sharing experiences, learning from others, and fostering a sense of belonging and empowerment.
Conclusion
In conclusion, type 1 diabetes presents unique challenges and complexities that distinguish it from type 2 diabetes. With its reliance on exogenous insulin, heightened risk of diabetic ketoacidosis, unpredictable blood sugar variability, and significant emotional and psychological impact, type 1 diabetes requires a comprehensive and multidisciplinary approach to management.
By providing individuals with type 1 diabetes and their families with education, support, and access to innovative technologies, we can empower them to navigate the challenges of diabetes and lead fulfilling and healthy lives. While type 1 diabetes may present formidable challenges, it also offers opportunities for resilience, growth, and advocacy within the diabetes community.
As our understanding of type 1 diabetes continues to evolve, ongoing research, innovation, and collaboration hold the promise of improving outcomes and transforming the lives of millions affected by this complex and impactful condition.