New research has revealed that diabetic retinopathy (DR), a major cause of vision loss, is far more common among those with diabetes than previously believed. Experts are urging for earlier and more frequent screenings to catch this condition before it leads to severe eye damage.
Diabetic retinopathy, which occurs when high blood sugar damages the blood vessels in the retina, was once thought to affect only a small percentage of individuals with type 1 and type 2 diabetes. However, a recent review published in the Journal of the American Medical Association (JAMA) found that nearly half of individuals with either type of diabetes experience some form of eye damage. Specifically, 52% of individuals with type 1 diabetes and 49% to 55% of those with type 2 diabetes showed signs of retinopathy. This starkly contrasts with earlier estimates, which suggested only 4% to 13% of people with diabetes had the condition.
Dr. Julie M. Rosenthal, a clinical assistant professor of ophthalmology at the University of Michigan, emphasized how this new data is changing the way experts view diabetic retinopathy. “This significantly shifts our understanding of the condition,” Dr. Rosenthal said, noting the surprising extent of eye damage found in young individuals with type 2 diabetes. Studies following young adults with either type 1 or type 2 diabetes found that after just seven years, more than half had developed diabetic retinopathy, with 3.5% experiencing macular edema, a serious complication.
The Growing Threat of Diabetic Retinopathy
Until now, many believed that children and adolescents with type 1 diabetes rarely developed retinopathy. However, this new data challenges that assumption, showing that even those diagnosed at a young age can be at risk for eye disease. Dr. Gillian Katz, an expert in endocrine services at NYC Health + Hospitals/Bellevue, explained that high blood sugar from diabetes can damage the blood vessels in the retina, leading to diabetic retinopathy, which can cause vision-threatening conditions like retinal detachment or fluid leakage into the retina.
Studies like the “TODAY” and “SEARCH” studies, which tracked young people with diabetes over several years, found that by the seven-year follow-up, over 50% of participants had developed some form of diabetic retinopathy. Surprisingly, individuals with type 2 diabetes were more likely to develop the disease earlier and in more severe forms compared to those with type 1 diabetes.
Given these findings, Dr. Rosenthal and other experts are questioning whether screening guidelines should be revised to begin earlier for people with diabetes, particularly those under 30.
Challenges in Detection
Diabetic retinopathy is often asymptomatic in its early stages, making it difficult to detect without regular eye exams. In many cases, the disease progresses without causing any noticeable changes in vision until more advanced stages, such as retinal detachment or internal bleeding. This delayed onset of symptoms underscores the importance of regular screenings, even for individuals who feel their vision is unaffected.
While blood sugar control can reduce the risk of diabetic retinopathy, even those with well-managed diabetes are not immune to the disease. Experts recommend that individuals with type 1 diabetes undergo a comprehensive eye exam within five years of diagnosis, while those with type 2 diabetes should do so immediately after diagnosis. However, these guidelines may need to be adjusted based on the new data suggesting higher rates of retinopathy among younger people.
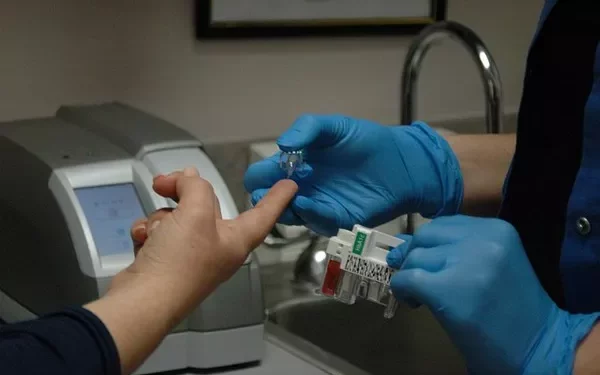
Current screening methods rely on visual assessments of the retina, but experts suggest that additional tests that measure retinal function could help detect the disease earlier, even before physical damage is visible.
The Role of AI in Early Detection
As access to eye care remains a challenge, especially in underserved communities, advancements in technology may offer a solution. AI-powered diagnostic tools like IDx-DR and EyeArt are already being used to detect diabetic retinopathy in primary care settings. These AI systems can identify signs of retinopathy in under a minute by analyzing images of the retina, offering a quick and reliable alternative to traditional screening methods.
Dr. Hunter Cherwek, an ophthalmologist with Orbis, believes that AI could revolutionize diabetic retinopathy screenings. “AI screening is a transformative tool that enhances early detection, improves access to care, and reduces the burden on ophthalmologists,” he said. AI technology has the potential to make screenings more accessible, especially in rural or low-resource settings, where shortages of ophthalmologists often make regular eye exams difficult.
The Path Forward
The prevalence of diabetic retinopathy in the U.S. has been steadily increasing, with approximately 9.6 million people now living with the condition. Experts predict that the number of people with diabetes will continue to grow, particularly among younger individuals. This trend presents an urgent need for better detection and treatment strategies to prevent vision loss.
Dr. Cherwek emphasized that the key to managing diabetic retinopathy lies in early detection. “Regular eye exams are critical for people with diabetes. Early detection can prevent blindness in up to 98% of cases,” he said.
With the advent of AI screening and improved awareness, experts are optimistic that diabetic retinopathy can be diagnosed earlier, preventing unnecessary vision loss and ensuring better long-term outcomes for people living with diabetes.
Related topics:
Managing Blood Sugar: Nutritionist Offers Key Tips to Control Diabetes
Diabetes Prevalence in Australia Could Be 35% Higher, New Study Finds