Managing blood sugar levels is a critical aspect of diabetes care, whether an individual is diagnosed with Type 1 diabetes, Type 2 diabetes, or is prediabetic. Understanding what constitutes a diabetic level of blood sugar is fundamental in both the prevention and management of this condition. It not only aids in making lifestyle adjustments but also helps in determining the effectiveness of treatment regimens and provides early warnings of possible complications.
Blood sugar, or blood glucose, is the main sugar found in the blood and serves as the body’s primary source of energy. When blood sugar levels are too high or too low, it can result in serious health complications. Maintaining optimal blood sugar levels is crucial for overall well-being. For individuals with diabetes, this becomes even more important as they may face challenges in managing their blood sugar effectively.
In this article, we will explore what constitutes a “diabetic level” of blood sugar, the factors influencing these levels, and how blood glucose levels are monitored. We will also discuss what actions need to be taken when blood sugar levels are out of the target range, as well as the long-term implications of poorly managed diabetes.
Understanding Blood Sugar Levels
Blood sugar levels fluctuate throughout the day depending on a variety of factors, including food intake, physical activity, medication, and stress. For individuals without diabetes, blood sugar levels are tightly regulated by the body’s natural insulin response. Insulin is a hormone produced by the pancreas that helps regulate blood glucose by facilitating its entry into cells where it is used for energy.
For those with diabetes, this regulation is impaired. Type 1 diabetes occurs when the pancreas produces little to no insulin, while Type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas doesn’t produce enough insulin to meet the body’s needs. In both cases, without proper management, blood glucose levels can rise to dangerously high levels, leading to complications.
Blood Sugar Levels: Normal vs. Diabetic
The first step in understanding what constitutes a diabetic level of blood sugar is knowing what is considered “normal” blood sugar. This can vary depending on the time of day and when food is consumed. Below are the general guidelines for healthy blood sugar levels:
1. Normal Blood Sugar Levels
Fasting Blood Sugar (Before Meals): 70-99 mg/dL (3.9-5.5 mmol/L)
Post-Meal (2 Hours After Eating): Less than 140 mg/dL (7.8 mmol/L)
HbA1c (Long-term Blood Glucose): Less than 5.7%
These values indicate that the body is able to regulate blood glucose effectively. For most people, maintaining these levels is relatively easy with a balanced diet, regular physical activity, and a healthy lifestyle.
2. Prediabetes Blood Sugar Levels
Individuals with prediabetes may have blood sugar levels that are higher than normal but not yet high enough to be diagnosed as diabetes. Prediabetes is a warning sign that diabetes is a possibility in the future. The following blood sugar readings are typically seen in individuals with prediabetes:
Fasting Blood Sugar: 100-125 mg/dL (5.6-6.9 mmol/L)
Post-Meal (2 Hours After Eating): 140-199 mg/dL (7.8-11.0 mmol/L)
HbA1c: 5.7-6.4%
A diagnosis of prediabetes provides an opportunity for intervention through lifestyle changes, such as improved diet and exercise, to prevent the onset of Type 2 diabetes.
3. Diabetes Blood Sugar Levels
For individuals diagnosed with diabetes, the blood sugar levels will typically exceed the normal range and require careful monitoring. The following blood glucose levels are indicative of diabetes:
Fasting Blood Sugar: 126 mg/dL (7.0 mmol/L) or higher
Post-Meal (2 Hours After Eating): 200 mg/dL (11.1 mmol/L) or higher
HbA1c: 6.5% or higher
These levels indicate that blood glucose is consistently elevated, and the individual may require medication, lifestyle changes, or both to manage their blood sugar and reduce the risk of complications.
Causes of Elevated Blood Sugar in Diabetes
When blood glucose levels become elevated, it is a sign that insulin is either not being produced in sufficient quantities (as in Type 1 diabetes) or that the body’s cells are not responding to insulin effectively (as in Type 2 diabetes). Several factors can contribute to this situation:
1. Insulin Resistance (Type 2 Diabetes)
In Type 2 diabetes, the body becomes resistant to the effects of insulin. This means that the insulin the pancreas produces is not as effective in lowering blood sugar levels. As a result, glucose builds up in the bloodstream, leading to elevated blood sugar levels. Over time, the pancreas may not be able to keep up with the increased demand for insulin.
2. Lack of Insulin (Type 1 Diabetes)
In Type 1 diabetes, the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. Without insulin, the body is unable to use glucose for energy, leading to high blood sugar levels. This is typically a lifelong condition that requires the individual to take insulin externally to regulate their blood sugar.
3. Diet and Lifestyle Factors
Diet plays a significant role in blood sugar regulation. Diets high in refined carbohydrates and sugars can cause rapid spikes in blood glucose, while poor diet choices may contribute to insulin resistance. Additionally, physical inactivity, obesity, and stress are all factors that can contribute to elevated blood sugar levels.
4. Medications
Certain medications can also affect blood sugar levels. For instance, corticosteroids and some diuretics may cause elevated blood sugar levels, while other medications are designed to lower blood sugar. It’s essential for individuals with diabetes to work closely with their healthcare provider to monitor and adjust their medication regimen as needed.
The Role of HbA1c in Monitoring Diabetes
In addition to blood glucose levels, healthcare providers often use HbA1c (glycated hemoglobin) to assess long-term blood sugar control. HbA1c measures the percentage of hemoglobin in the blood that is coated with sugar, providing a three-month average of blood glucose levels. It is a critical tool in diagnosing and managing diabetes.
Normal HbA1c: Below 5.7%
Prediabetes HbA1c: 5.7-6.4%
Diabetes HbA1c: 6.5% or higher
By regularly measuring HbA1c, individuals and healthcare providers can assess how well blood sugar levels have been controlled over time, helping to guide treatment decisions and adjust lifestyle recommendations.
Monitoring Blood Sugar Levels
Blood sugar levels fluctuate throughout the day, so it’s important for individuals with diabetes to regularly monitor their blood glucose to ensure it stays within a target range. Monitoring is essential for preventing hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar), both of which can lead to serious complications.
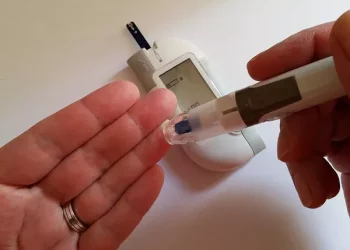
1. Self-Monitoring of Blood Glucose (SMBG)
Individuals with diabetes can monitor their blood glucose levels at home using a blood glucose meter. This involves pricking the finger to obtain a small blood sample, which is then tested using a glucose strip. The results provide immediate feedback on the individual’s blood sugar levels and can help guide dietary, medication, and lifestyle decisions.
2. Continuous Glucose Monitoring (CGM)
For individuals with Type 1 diabetes or those with Type 2 diabetes who have difficulty maintaining stable blood sugar levels, continuous glucose monitoring (CGM) is a valuable tool. CGM devices track blood sugar levels continuously throughout the day and night, providing real-time data on fluctuations in blood glucose levels. This information can help individuals make adjustments to their diet, exercise, and medication in real time.
3. Target Blood Sugar Ranges
While the specific target blood sugar range may vary depending on an individual’s health goals, treatment plan, and other factors, the general targets for people with diabetes are as follows:
Fasting Blood Sugar: 80-130 mg/dL (4.4-7.2 mmol/L)
Post-Meal Blood Sugar (2 Hours After Eating): Less than 180 mg/dL (10.0 mmol/L)
HbA1c: Less than 7%
By regularly monitoring blood glucose levels and staying within these target ranges, individuals with diabetes can reduce their risk of long-term complications, such as heart disease, kidney damage, nerve damage, and vision loss.
When to Seek Medical Help
Managing blood sugar effectively is essential for maintaining health and preventing complications. However, there are times when it may be necessary to seek medical help:
High Blood Sugar (Hyperglycemia): If blood sugar levels exceed 300 mg/dL (16.7 mmol/L) or higher, it may indicate an emergency, especially if accompanied by symptoms like frequent urination, extreme thirst, blurred vision, or fatigue.
Low Blood Sugar (Hypoglycemia): If blood sugar levels drop below 70 mg/dL (3.9 mmol/L), it can lead to confusion, dizziness, sweating, shakiness, or even loss of consciousness. This requires immediate intervention, typically through the consumption of glucose or other fast-acting carbohydrates.
Conclusion
Understanding diabetic levels of blood sugar is fundamental to effectively managing diabetes and preventing the onset of complications. By regularly monitoring blood glucose levels, making lifestyle adjustments, and working with healthcare providers, individuals with diabetes can maintain control over their blood sugar and improve their overall health. Early intervention, regular monitoring, and adherence to treatment plans can make a significant difference in the lives of individuals living with diabetes, allowing them to lead healthier, more fulfilling lives.
Related topics: