The concept of monitoring blood glucose levels is central to managing diabetes and preventing complications. One of the key measures in assessing overall blood sugar control is the HbA1c test, also known as the glycated hemoglobin test. This test provides a snapshot of a person’s average blood sugar level over the past two to three months and plays a crucial role in guiding treatment decisions for people with diabetes.
This article explores the significance of the A1C test, the ideal range for A1C levels, and the factors influencing what constitutes a “perfect” A1C reading. Through an evidence-based approach, we will examine how individuals with diabetes can achieve optimal blood glucose control and understand how the A1C test fits into their overall treatment plan.
What Is HbA1c?
Hemoglobin is a protein found in red blood cells that helps carry oxygen throughout the body. When glucose (sugar) enters the bloodstream, some of it binds to hemoglobin, forming glycated hemoglobin (HbA1c). The higher the blood glucose levels over time, the more glucose binds to the hemoglobin, increasing the HbA1c level.
The A1C test measures the percentage of hemoglobin molecules in the blood that are coated with glucose. The result is a percentage, which reflects how well blood sugar has been controlled over the previous two to three months.
The Importance of the A1C Test in Diabetes Management
The A1C test is widely used because it offers a long-term picture of blood sugar control, rather than the fluctuations that might occur throughout the day. For individuals with diabetes, maintaining their A1C within a target range is critical for preventing both short- and long-term complications, such as nerve damage, kidney disease, heart disease, and vision problems.
For those who are not diabetic, normal A1C levels suggest that their blood sugar levels are well-regulated. It’s important to note, however, that the A1C test should be interpreted alongside other factors, such as blood glucose levels, medical history, and the presence of any comorbidities.
Understanding A1C Targets
In diabetes care, A1C targets vary depending on the individual’s circumstances, including their age, the duration of diabetes, the presence of other health conditions, and the specific type of diabetes they have. In general, a lower A1C is associated with better blood glucose control and fewer complications.
The American Diabetes Association (ADA) generally recommends the following A1C targets:
For the general population with diabetes: An A1C level of less than 7%.
For older adults or those with comorbidities: An A1C target of around 7.5% to 8% may be appropriate, as more aggressive control may increase the risk of hypoglycemia.
For children and adolescents: The target A1C is typically less than 7.5%, but age and individual circumstances should be taken into account.
For pregnant women: The target should generally be below 6.5%, as high blood glucose during pregnancy can increase the risk of complications for both the mother and baby.
What Is the Perfect A1C?
The “perfect” A1C reading, while commonly viewed as below 6.5%, is not a one-size-fits-all number. The ideal target depends on multiple factors, including a person’s overall health, age, lifestyle, and the type of diabetes they have. For some individuals, a target below 7% may be optimal for preventing complications, while for others, a slightly higher target may be more appropriate to avoid the risks associated with hypoglycemia.
For individuals with Type 1 or Type 2 diabetes, achieving an A1C level as close to normal as possible—without experiencing dangerous lows—is a key goal. However, it is essential to understand that achieving an A1C level that is too low (especially below 6%) may pose a risk for hypoglycemia, particularly for those on insulin or other blood sugar-lowering medications.
Ideal A1C for Type 1 Diabetes
For individuals with Type 1 diabetes, the goal is to keep blood sugar levels within a target range that minimizes the risk of complications, including diabetic retinopathy, nephropathy, and neuropathy. The A1C target for most individuals with Type 1 diabetes is less than 7%, although this target should be adjusted based on the person’s age, health status, and other individual factors.
It’s important to remember that Type 1 diabetes is a chronic condition where the body’s ability to produce insulin is impaired, meaning blood sugar regulation must be closely monitored through frequent blood glucose checks and insulin adjustments.
Ideal A1C for Type 2 Diabetes
For individuals with Type 2 diabetes, the goals of treatment also aim at reducing the risk of long-term complications while avoiding the potential dangers of low blood sugar. An A1C of less than 7% is commonly recommended for adults with Type 2 diabetes who are otherwise healthy.
However, for older adults or individuals with multiple comorbidities or a history of hypoglycemia, a slightly higher target, such as 7.5% to 8%, may be considered to prevent overly aggressive treatment and reduce the risk of adverse effects.
Factors That Affect A1C Readings
While maintaining blood glucose levels within a target range is essential for a good A1C, several factors can affect A1C readings, making it crucial to understand the nuances of this test.
Blood Glucose Patterns
A person’s daily blood glucose patterns—whether they experience frequent highs or lows—will influence their A1C reading. If blood glucose levels tend to be high after meals but controlled in the morning, this may result in an elevated A1C, even if the person is otherwise maintaining good blood sugar control.
Hemoglobin Variations
Certain variations in hemoglobin can lead to inaccurate A1C readings. Individuals with anemia or other blood disorders, such as sickle cell anemia, may have altered hemoglobin, leading to falsely low or high A1C levels. In these cases, other methods of monitoring blood glucose, such as continuous glucose monitoring (CGM), may be more accurate.
Age and Health Conditions
As individuals age, their body’s ability to regulate blood sugar naturally declines. For this reason, older adults may be at greater risk of having a higher A1C level. In addition, people with other health conditions, such as chronic kidney disease or liver disease, may experience higher-than-normal A1C readings.
Medication Use
The medications that a person with diabetes is taking can influence their A1C level. Insulin therapy, for instance, is designed to lower blood sugar levels, thus affecting A1C readings. However, overuse of insulin or other glucose-lowering medications can increase the risk of hypoglycemia, which should be carefully monitored.
How to Achieve a Healthy A1C
Achieving a healthy A1C requires a multifaceted approach. Here are several strategies that can help individuals with diabetes control their blood sugar levels and lower their A1C:
Diet and Nutrition: Eating a balanced diet that is rich in whole foods, such as vegetables, whole grains, lean proteins, and healthy fats, is crucial for blood sugar control. Monitoring carbohydrate intake is particularly important, as carbs directly affect blood sugar levels.
Regular Exercise: Physical activity helps the body use insulin more effectively, which can lower blood glucose levels and improve A1C. A combination of aerobic exercise (such as walking, jogging, or swimming) and strength training can offer the best results.
Medication Management: For many individuals with diabetes, medication is a key component of treatment. Oral medications, insulin, and other injectables can help control blood sugar levels and keep A1C within the target range. It’s important to work with a healthcare provider to adjust medications as needed.
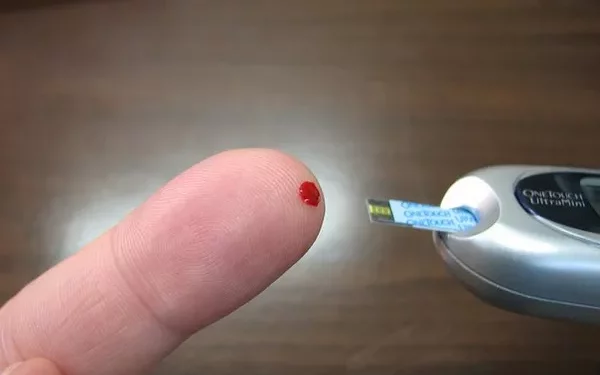
Monitoring Blood Sugar: Regular blood glucose monitoring provides valuable feedback about how well blood sugar is controlled throughout the day. For some individuals, continuous glucose monitoring (CGM) can offer real-time data and help detect trends that may require intervention.
Stress Management: Stress can elevate blood glucose levels by increasing the release of stress hormones, such as cortisol. Managing stress through mindfulness, meditation, yoga, and other relaxation techniques can help keep blood sugar levels stable.
Adequate Sleep: Sleep deprivation can disrupt insulin sensitivity and blood sugar regulation, leading to higher-than-normal A1C levels. Ensuring sufficient and restful sleep each night is an important part of diabetes management.
Regular Health Check-ups: Regular visits to a healthcare provider help monitor overall health and make adjustments to treatment plans as needed. Providers can help individuals set realistic A1C targets based on their health status and progress.
Conclusion
The “perfect” A1C reading is highly individual and should be tailored to each person’s health status, treatment goals, and risk factors. While an A1C of less than 7% is often considered ideal, achieving the right target depends on factors such as age, comorbidities, and the type of diabetes one has. Individuals with diabetes must work closely with their healthcare providers to determine the best target range for their specific situation and take a proactive approach to managing their blood glucose levels.
In the end, the perfect A1C reading is not just a number—it is the result of a comprehensive, personalized diabetes management plan that includes lifestyle changes, medication, monitoring, and consistent healthcare support. By striving for balance and focusing on long-term health goals, people with diabetes can reduce their risk of complications and enjoy a better quality of life.
Related topics: