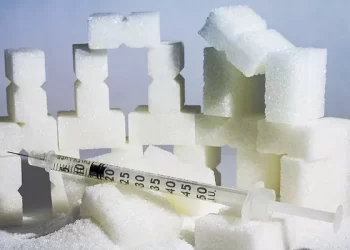
Blood glucose monitoring is a cornerstone of diabetes management. Whether you’re living with diabetes, at risk for it, or simply interested in understanding how your body processes sugar, knowing what constitutes a “normal” blood glucose reading is essential. However, the term “normal” can vary depending on factors like timing, the type of test being used, and individual health conditions. But what does it truly mean for a blood glucose reading to be “accurate,” and how can you ensure that the readings you are getting are reliable?
In this article, we’ll break down the factors that contribute to accurate blood glucose readings, including what a “normal” level looks like, the importance of timing and technology, and how you can make sure your readings provide the insights you need for effective management.
Understanding Blood Glucose
Blood glucose is the amount of sugar present in your bloodstream. It serves as the body’s primary energy source and is regulated by insulin, a hormone secreted by the pancreas. If your blood glucose levels are too high (hyperglycemia) or too low (hypoglycemia), your body can experience immediate symptoms and, over time, develop complications.
What Influences Blood Glucose Levels?
Blood glucose levels fluctuate throughout the day, influenced by several factors:
Diet: Carbohydrates, especially sugars, impact blood glucose levels. Fast-digesting carbs can cause quick spikes, while fiber-rich foods slow the process.
Exercise: Physical activity helps muscles utilize glucose more effectively, typically lowering blood sugar levels.
Stress and Illness: Hormonal changes during stress or illness can elevate glucose levels.
Medications: Certain medications (including insulin and steroids) can affect blood glucose levels.
Sleep and Circadian Rhythm: Glucose levels naturally fluctuate based on the body’s circadian rhythm, and sleep deprivation can affect insulin sensitivity.
Thus, blood glucose readings must be considered in the context of these variables for a true understanding of a person’s health status.
What Is a Normal Blood Glucose Reading?
When we refer to a “normal” blood glucose reading, it typically implies values that are considered safe and healthy for an individual, usually outside the threshold for conditions like diabetes or prediabetes.
Fasting Blood Glucose
A fasting blood glucose test measures blood sugar levels after a person has fasted for at least 8 hours (usually overnight). This test is often used for diagnosing diabetes or monitoring glucose control.
Normal Fasting Glucose: 70 to 99 mg/dL (3.9 to 5.5 mmol/L)
Prediabetes (Impaired Fasting Glucose): 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
Diabetes: 126 mg/dL (7.0 mmol/L) or higher, confirmed on two separate tests
Postprandial (After Meal) Blood Glucose
Postprandial readings are taken 2 hours after eating, and they reflect how effectively the body is managing the glucose from the consumed food.
Normal: Less than 140 mg/dL (7.8 mmol/L)
Prediabetes: 140 to 199 mg/dL (7.8 to 11.0 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher
Random Blood Glucose
Random blood glucose tests are taken at any time of the day, regardless of meals.
Normal: Less than 140 mg/dL (7.8 mmol/L)
Diabetes: 200 mg/dL (11.1 mmol/L) or higher, along with symptoms of diabetes, is diagnostic.
Glycated Hemoglobin (HbA1c)
The HbA1c test measures your average blood glucose level over the past 2 to 3 months. It’s another useful tool for assessing long-term glucose control, particularly for individuals with diabetes.
Normal HbA1c: Less than 5.7%
Prediabetes: 5.7% to 6.4%
Diabetes: 6.5% or higher
Ensuring Accurate Blood Glucose Readings
An accurate blood glucose reading depends on several factors, ranging from the method of measurement to how the test is conducted. Below, we will outline the most significant factors to consider when aiming for accurate results.
Type of Test Used
The type of test you use to measure your blood glucose levels can significantly impact the accuracy of the readings. There are several methods available:
Home Glucose Meters (Glucometers)
Home glucose meters are the most common tool for measuring blood glucose at home. They are portable, easy to use, and provide quick results. However, to get an accurate reading, consider the following:
Calibration: Glucometers must be calibrated to ensure accuracy. Always follow manufacturer instructions for proper calibration and maintenance.
Blood Sample Quality: A small drop of blood is required for testing, and contamination (such as from food residue or improper cleaning of the testing site) can impact results.
Testing Conditions: Ensure you are in a comfortable, relaxed environment. Stress, extreme temperatures, or a poorly prepared sample may skew results.
Continuous Glucose Monitors (CGMs)
CGMs are advanced devices that provide continuous monitoring of blood glucose levels throughout the day and night. These devices are worn on the body and use a sensor inserted just under the skin to measure glucose levels in the interstitial fluid. While CGMs provide valuable insights, they are generally considered less accurate than direct blood glucose meters, particularly in cases of rapidly changing glucose levels.
To optimize accuracy with CGMs:
-
Calibrate regularly if required by the device.
-
Ensure proper placement of the sensor on a clean, dry area of the skin.
-
Monitor sensor performance for any signs of malfunction or poor data quality.
Laboratory Tests
Laboratory tests, like fasting glucose or HbA1c, are typically more accurate than at-home meters. They involve drawing a blood sample at a healthcare facility and analyzing it with more sophisticated equipment. These tests are essential for establishing diagnoses, particularly in the context of diabetes or prediabetes.
Timing of the Test
Blood glucose levels naturally fluctuate throughout the day, so timing is crucial for an accurate reading. For instance:
Morning readings: Many people experience a higher blood glucose reading in the morning due to the body’s natural hormonal rhythm, which can increase glucose production. This is called the “dawn phenomenon.”
Post-meal readings: Testing blood glucose levels 2 hours after eating gives the most accurate representation of how well your body is managing glucose from food.
Before bed: Some people test before going to sleep to see how their glucose levels are stabilizing after meals and exercise throughout the day.
Proper Technique and Hygiene
The accuracy of a blood glucose reading is greatly affected by the technique used:
Wash your hands thoroughly before testing to avoid contaminants that may affect the result.
Use a proper lancet device to obtain a blood sample, ensuring it’s clean and not too deep to avoid excess tissue damage.
Avoid squeezing the finger after pricking it, as this can contaminate the blood sample with interstitial fluid.
Environmental Factors
External factors such as temperature, humidity, and even altitude can influence the accuracy of blood glucose meters. Most glucose meters are calibrated for use in normal room temperature ranges (between 59–86°F or 15–30°C). Testing in extreme conditions, such as freezing cold or very hot temperatures, may lead to inaccurate results.
What to Do When Your Reading Is Outside the Normal Range
Understanding how to interpret abnormal readings is crucial for managing your health. Here’s what to do when you encounter a result that falls outside the normal range.
High Readings (Hyperglycemia)
High blood glucose readings may signal several things:
Poor diabetes control: If your readings are consistently high, it may mean that your insulin dosage or management plan needs adjustment.
Illness or stress: Physical stressors, such as infections or injury, can raise blood glucose levels.
Dietary factors: Consuming high-glycemic foods or large meals may cause spikes in blood glucose.
If you have a high reading, it is essential to monitor your condition, drink plenty of water, and avoid further high-sugar foods. If the reading is significantly elevated (over 250–300 mg/dL), you may need to seek medical attention or adjust your medication regimen.
Low Readings (Hypoglycemia)
Hypoglycemia occurs when blood glucose falls below 70 mg/dL. It is common among individuals who are on insulin or other blood sugar-lowering medications. Symptoms can include shakiness, dizziness, confusion, and sweating. If your reading is low:
Consume fast-acting carbohydrates, like glucose tablets, juice, or regular soda.
Recheck your glucose levels after 15 minutes to ensure it’s rising.
Avoid overcorrecting by consuming too much sugar, which can lead to a rebound hyperglycemia.
When to Seek Medical Help
Consistent abnormal readings—whether high or low—require medical attention. If you’re managing diabetes, it’s essential to work with your healthcare provider to establish a tailored plan for blood glucose control. Additionally, if you experience symptoms such as persistent nausea, vomiting, or signs of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), seek emergency medical care immediately.
Conclusion:
A normal, accurate blood glucose reading is crucial for diagnosing and managing diabetes and other metabolic conditions. Regular monitoring, proper testing techniques, and understanding what influences glucose levels are key factors in ensuring reliable results.
By understanding what is considered “normal,” how to achieve accurate readings, and how to interpret and respond to your glucose levels, you can maintain optimal health and minimize complications. Whether you’re managing diabetes, prediabetes, or simply trying to maintain a healthy lifestyle, accurate blood glucose readings are vital to making informed decisions about your health.
Related topics:
What Causes High Glucose Levels?