Gestational diabetes, a condition affecting pregnant women, poses significant health risks to both mothers and their babies, requiring careful monitoring and treatment. However, a growing body of research indicates that women of color are more likely to be diagnosed with this condition, raising concerns about potential health inequities.
Dr. Gabrielle Cassir, a maternal-fetal medicine specialist at McGill University, explains that gestational diabetes occurs when the body cannot produce enough insulin to overcome the insulin resistance brought on by pregnancy. While factors such as age, family medical history, and pre-pregnancy obesity can increase a woman’s risk, ethnicity also plays a significant role.
In Canada, approximately 7.9% of pregnant women are diagnosed with gestational diabetes, with global figures rising to 17%. In North America, the prevalence is around 10%, and Southeast Asia sees rates as high as 25%. Research suggests that certain ethnic groups, including Hispanic, Native American, Alaskan, Native Hawaiian, and South or East Asian populations, have a higher incidence of gestational diabetes due to a greater prevalence of type 2 diabetes within these communities.
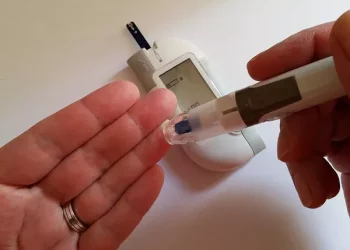
The screening process for gestational diabetes typically involves a glucose tolerance test. In Canada, the process begins with a 50-gram glucose drink, followed by a second, more comprehensive 75-gram test if results fall into the “gray zone.” Those who fail the test are diagnosed and closely monitored throughout their pregnancy, often requiring additional visits, nutritional guidance, and regular ultrasounds.
Women with gestational diabetes face an increased risk of complications, including preeclampsia, large-for-gestational-age babies, and cesarean deliveries. Post-birth, their babies are tested for issues such as hypoglycemia, jaundice, and respiratory distress. Mothers are also advised to undergo follow-up screenings for type 2 diabetes, as gestational diabetes significantly increases their long-term risk.
Dr. Kaberi Dasgupta, a professor of medicine at McGill, highlights that while genetics and family history play a significant role in gestational diabetes risk, social and historical factors—such as the legacy of colonization and slavery—can exacerbate the condition among Black populations. These socio-historical factors, combined with modern-day factors like sedentary lifestyles and poor dietary habits, can lead to epigenetic changes that make the body more efficient at processing sugars and calories. These changes may persist across generations, further contributing to health disparities.
Despite the evidence of these disparities, Dr. Dasgupta cautions against altering the diagnostic thresholds for gestational diabetes based on ethnicity alone. While there is a need to account for these factors in patient care, she emphasizes that a one-size-fits-all approach may not be feasible yet, as the condition and its complexities continue to evolve.
Overall, the connection between ethnicity, socio-economic conditions, and the diagnosis of gestational diabetes reveals a pressing need for targeted health interventions and further research to address these disparities and improve outcomes for all expectant mothers.
Related topics:
Diabetes Drug Shows Promise in Reducing Heart Failure Risk for Cancer Survivors
Shorter Glucose Test Shows Stronger Prediction of Diabetes Risk
Novel Strategy Aims to Halt Beta Cell Damage in Type 2 Diabetes