Diabetes is a chronic condition that affects millions of people worldwide. It is characterized by high blood sugar levels that can lead to serious complications such as heart disease, kidney failure, nerve damage, and even vision loss. However, not all individuals with elevated blood sugar levels have full-blown diabetes. A condition known as prediabetes or borderline diabetes exists, where blood sugar levels are higher than normal but not yet high enough to meet the diagnostic criteria for diabetes. Understanding the sugar level that constitutes borderline diabetes is crucial for early detection and intervention to prevent the progression to type 2 diabetes.
In this article, we will explore the concept of borderline diabetes, the diagnostic criteria used to assess blood sugar levels, and the steps individuals can take to manage their condition and prevent the onset of type 2 diabetes.
What Is Borderline Diabetes?
Borderline diabetes, often referred to as prediabetes, is a condition in which blood sugar levels are elevated, but not to the extent that they qualify as diabetes. This stage is a critical point in diabetes progression and offers an opportunity for intervention. Without lifestyle changes, however, those with borderline diabetes are at a much higher risk of developing type 2 diabetes within five to ten years.
Prediabetes is often asymptomatic, meaning that individuals may not feel unwell or notice any significant changes in their health. For this reason, it is referred to as the “silent” stage of diabetes. The condition can only be detected through blood tests that measure glucose levels in the blood.
Diagnostic Criteria for Borderline Diabetes
Borderline diabetes is diagnosed through specific blood sugar tests. The main tests used to assess blood sugar levels are:
- Fasting Blood Sugar Test (FBS)
- Oral Glucose Tolerance Test (OGTT)
- Hemoglobin A1c Test (HbA1c)
Each of these tests provides different insights into how well the body is managing blood sugar. The results of these tests are used to determine whether an individual has normal glucose levels, borderline diabetes, or full-blown diabetes.
1. Fasting Blood Sugar (FBS)
The fasting blood sugar test measures the amount of glucose in your blood after fasting for at least eight hours. This test is commonly used to diagnose prediabetes or diabetes, as it gives an indication of how well your body manages glucose after an overnight fast.
- Normal Range: 70 to 99 mg/dL (milligrams per deciliter)
- Prediabetes (Borderline Diabetes): 100 to 125 mg/dL
- Diabetes: 126 mg/dL or higher on two separate occasions
If your fasting blood sugar is between 100 and 125 mg/dL, it means you have borderline diabetes or prediabetes. If your blood sugar exceeds 126 mg/dL, you may be diagnosed with type 2 diabetes.
2. Oral Glucose Tolerance Test (OGTT)
The oral glucose tolerance test is a more involved procedure. It measures how well your body processes glucose after drinking a sugary solution. It is typically used when a fasting blood sugar test shows borderline results, or when a more precise diagnosis is required.
- Normal Range: Less than 140 mg/dL two hours after drinking the glucose solution
- Prediabetes (Borderline Diabetes): 140 to 199 mg/dL two hours after drinking the glucose solution
- Diabetes: 200 mg/dL or higher two hours after drinking the glucose solution
The OGTT is particularly useful for identifying individuals with elevated blood sugar levels who may not show abnormal results on a fasting blood sugar test but still have impaired glucose tolerance.
3. Hemoglobin A1c Test (HbA1c)
The hemoglobin A1c test measures the average blood sugar level over the past two to three months. It reflects how well blood sugar levels have been controlled over time and is often used to diagnose diabetes and prediabetes.
- Normal Range: Below 5.7%
- Prediabetes (Borderline Diabetes): 5.7% to 6.4%
- Diabetes: 6.5% or higher
The HbA1c test does not require fasting and is a more comprehensive test, as it reflects long-term blood sugar control. For individuals with prediabetes, a HbA1c between 5.7% and 6.4% is considered an indication of borderline diabetes.
Why Blood Sugar Levels Matter
Blood sugar (glucose) is the body’s primary energy source, derived from the food we consume. After eating, food is broken down into glucose, which is then absorbed into the bloodstream. The pancreas releases insulin, a hormone that helps cells absorb glucose for energy. In people with prediabetes, the body begins to resist insulin’s effects, causing glucose to build up in the bloodstream instead of being absorbed into cells.
When blood sugar levels are consistently elevated, even in the prediabetes range, it can lead to serious health consequences, including damage to blood vessels, nerves, and organs. However, the body may still function relatively normally in the early stages, which is why many people do not recognize the signs of borderline diabetes.
Who Is at Risk of Borderline Diabetes?
Several factors can increase the likelihood of developing borderline diabetes. These risk factors include:
Age: People over the age of 45 are at higher risk, especially if they are overweight or sedentary.
Family History: A family history of type 2 diabetes increases the risk of developing prediabetes.
Obesity: Excess body fat, particularly abdominal fat, increases the risk of insulin resistance, a precursor to prediabetes.
Physical Inactivity: A lack of physical activity can lead to weight gain and insulin resistance, increasing the likelihood of developing prediabetes.
Poor Diet: A diet high in processed foods, refined carbohydrates, and sugary drinks can contribute to elevated blood sugar levels.
High Blood Pressure or Abnormal Cholesterol Levels: People with hypertension or abnormal lipid levels are more likely to develop prediabetes.
Gestational Diabetes: Women who have had gestational diabetes during pregnancy are at a higher risk of developing prediabetes later in life.
How to Prevent or Reverse Borderline Diabetes
The good news is that borderline diabetes is reversible with lifestyle changes. If blood sugar levels are elevated but not yet high enough to meet the criteria for type 2 diabetes, taking action now can prevent the progression to full-blown diabetes. Here are several key strategies to manage and potentially reverse borderline diabetes:
1. Lose Excess Weight
Losing even a small amount of weight can have a significant impact on blood sugar levels. Studies show that losing 5-10% of your body weight can improve insulin sensitivity and lower blood glucose levels. Achieving and maintaining a healthy weight through a combination of diet and exercise is one of the most effective ways to reverse prediabetes.
2. Increase Physical Activity
Regular physical activity helps the body use insulin more efficiently and lowers blood sugar levels. Aim for at least 150 minutes of moderate aerobic exercise, such as brisk walking or swimming, per week. Resistance training, such as weightlifting or bodyweight exercises, can also help build muscle mass and improve insulin sensitivity.
3. Follow a Healthy Diet
A balanced diet is essential for managing blood sugar levels. Focus on consuming whole grains, lean proteins, healthy fats, and a variety of fruits and vegetables. Limit processed foods, sugary drinks, and foods high in refined carbohydrates, as they can cause blood sugar spikes.
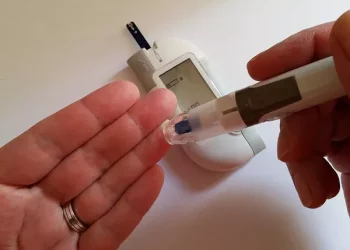
4. Monitor Blood Sugar Regularly
For those with borderline diabetes, monitoring blood sugar regularly can help track progress and identify trends. While it may not be necessary for everyone with prediabetes, some individuals may benefit from regular blood glucose testing to gauge how well their lifestyle changes are working.
5. Manage Stress
Chronic stress can lead to elevated blood sugar levels and insulin resistance. Practice stress-reducing techniques such as yoga, meditation, deep breathing exercises, or spending time in nature. Getting adequate sleep each night is also important for stress management and overall health.
6. Medications
In some cases, a healthcare provider may recommend medications to help control blood sugar levels. The most commonly prescribed medication for prediabetes is metformin, which helps lower glucose production in the liver and improves insulin sensitivity.
Conclusion: Borderline Diabetes Is a Warning Sign
Borderline diabetes, or prediabetes, is a critical stage in the development of type 2 diabetes. It is characterized by blood sugar levels that are higher than normal but not yet high enough to meet the criteria for a diabetes diagnosis. While borderline diabetes is often asymptomatic, it is a warning sign that should not be ignored.
Regular blood sugar testing, along with lifestyle changes such as losing weight, increasing physical activity, and following a healthy diet, can help reverse prediabetes and prevent the onset of type 2 diabetes. For those diagnosed with borderline diabetes, taking action now is key to managing the condition and avoiding long-term complications. By addressing risk factors and making healthier choices, individuals can regain control of their health and prevent the progression to full-blown diabetes.
Related topics:
What’s Your Target Glucose Range