Blood sugar regulation is at the core of diabetes management, as both high and low blood sugar levels (hyperglycemia and hypoglycemia, respectively) can lead to significant health complications. Among the more immediate and concerning risks for people with diabetes is hypoglycemia, or low blood sugar. Hypoglycemia can occur suddenly and without warning, and recognizing its symptoms early is crucial for preventing serious health issues, such as fainting, seizures, or even loss of consciousness.
For individuals with diabetes, especially those who are on insulin therapy or certain oral medications, learning to recognize the signs of low blood sugar and understanding the steps needed to address it is vital. This article aims to provide a comprehensive overview of how to identify when your blood sugar is low, the causes and symptoms of hypoglycemia, and how to manage and prevent low blood sugar episodes.
What Is Hypoglycemia?
Hypoglycemia refers to a condition where your blood sugar levels drop too low, typically below 70 mg/dL (3.9 mmol/L). In some cases, hypoglycemia may occur even when blood sugar levels are slightly higher, depending on the individual’s usual blood sugar levels and sensitivity to insulin. While hypoglycemia can occur in anyone, it is most common in people with diabetes who are managing their condition with insulin or medications that increase insulin production.
The symptoms of low blood sugar can range from mild to severe and vary from person to person. Recognizing these symptoms early and responding appropriately can help prevent more severe consequences, such as confusion, loss of consciousness, or even coma.
Causes of Low Blood Sugar in People with Diabetes
There are several common causes of hypoglycemia for people with diabetes:
Excessive Insulin or Diabetes Medication: The most common cause of hypoglycemia in people with diabetes is taking too much insulin or certain diabetes medications, such as sulfonylureas (which stimulate the pancreas to release more insulin). Overdosing on insulin or medication can lead to an excessive drop in blood sugar levels.
Skipping Meals or Eating Less: If you skip a meal, delay eating, or don’t consume enough carbohydrates, your body may not have enough glucose available to maintain stable blood sugar levels. This can lead to a drop in blood sugar, especially if you’ve taken insulin or other blood sugar-lowering medications before the missed or delayed meal.
Increased Physical Activity: Exercise or physical activity causes muscles to use more glucose for energy. If you don’t adjust your insulin doses or eat extra carbohydrates before exercise, the increase in physical activity can cause your blood sugar to drop too low.
Alcohol Consumption: Drinking alcohol, especially without food, can interfere with the liver’s ability to release glucose into the bloodstream, which can result in low blood sugar levels. This is particularly dangerous for people with diabetes who use insulin or medications that increase insulin production.
Illness or Infection: During illness or infection, the body’s stress response can affect how insulin works and how glucose is processed. Additionally, people with diabetes may eat less or experience changes in eating habits when ill, increasing the likelihood of hypoglycemia.
Dehydration: Being dehydrated can alter blood sugar control, and when you are dehydrated, your blood sugar levels can fluctuate more than usual, potentially increasing the risk of hypoglycemia.
Symptoms of Low Blood Sugar: How to Recognize It
Hypoglycemia symptoms can vary widely, and some individuals may experience only a few symptoms, while others may experience a range of them. Generally, hypoglycemia symptoms are divided into early warning signs (mild symptoms) and severe symptoms (when blood sugar is dangerously low).
1. Early Warning Signs of Low Blood Sugar
These early symptoms of low blood sugar may occur when your blood sugar level starts to drop but has not yet reached a critical level:
Shakiness: A common early sign of hypoglycemia is feeling shaky or jittery, often accompanied by nervousness or anxiety. This occurs as the body’s fight-or-flight response is triggered.
Sweating: Profuse sweating, particularly when it is out of proportion to the environmental temperature, can signal a drop in blood sugar.
Heart Palpitations: Some individuals may experience a racing heart or feel as though their heart is pounding in their chest due to the release of adrenaline in response to low blood sugar.
Hunger: Intense feelings of hunger, often accompanied by a craving for sweets or carbohydrates, are a common symptom of hypoglycemia.
Dizziness or Lightheadedness: Low blood sugar can cause a feeling of dizziness or faintness, particularly when standing up or moving suddenly.
Fatigue: A sudden feeling of fatigue or weakness, even after a full night of sleep, is another sign that your blood sugar may be low.
Irritability: Changes in mood, such as irritability or sudden emotional outbursts, can be a result of low blood sugar. This is due to the brain’s reduced glucose supply, which can affect emotional regulation.
Headache: A headache may occur as a result of low glucose levels, often accompanied by a general feeling of unwellness.
Blurry Vision: Low blood sugar levels can affect the eyes, leading to temporary blurry vision or difficulty focusing.
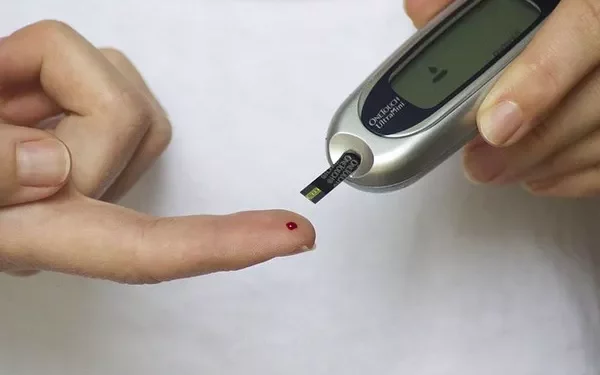
If you begin to experience any of these symptoms, it’s important to test your blood sugar immediately using a glucose meter to determine if your blood sugar is indeed low.
2. Severe Symptoms of Low Blood Sugar
If low blood sugar goes unaddressed, symptoms can escalate and become severe. This can lead to confusion, loss of consciousness, or even seizures. The symptoms of severe hypoglycemia include:
Confusion or Difficulty Concentrating: When blood sugar levels drop too low, it can affect brain function, leading to confusion, difficulty speaking, or trouble understanding simple instructions.
Unusual Behavior or Personality Changes: People with severe hypoglycemia may exhibit strange behaviors, such as acting irrationally, becoming combative, or making poor decisions.
Loss of Coordination: Severe hypoglycemia can cause a loss of motor coordination, making it difficult to walk, balance, or even stand up.
Seizures: Extremely low blood sugar can lead to seizures, which occur when the brain’s glucose supply is critically insufficient.
Loss of Consciousness: If blood sugar levels drop dangerously low, a person may lose consciousness or even slip into a hypoglycemic coma. This is a medical emergency and requires immediate intervention.
Coma: In rare, severe cases, hypoglycemia can lead to a coma, especially if it is untreated for a long period.
If you experience any of the severe symptoms of hypoglycemia, seek medical help immediately. If you are unable to treat the low blood sugar yourself or are in a situation where you cannot consume glucose, emergency services should be called.
How to Manage Low Blood Sugar
The key to managing low blood sugar is recognizing it early and taking action immediately. Here’s what you can do to address low blood sugar levels:
1. Treating Mild Hypoglycemia
If your blood sugar reading is below 70 mg/dL and you’re experiencing early warning signs of hypoglycemia, the treatment is relatively straightforward:
Consume fast-acting carbohydrates: The goal is to quickly raise your blood sugar levels to a safe range. Choose fast-acting carbohydrates such as:
- Glucose tablets (typically 15 grams of carbohydrates)
- 4 ounces (about half a cup) of fruit juice
- 1 tablespoon of honey or sugar
- 5 to 6 hard candies (that are not sugar-free)
Wait 15 minutes: After consuming the fast-acting carbohydrates, wait about 15 minutes to allow your body to process the sugar.
Check your blood sugar again: After waiting 15 minutes, check your blood sugar level again. If it is still below 70 mg/dL, repeat the treatment. If your blood sugar has returned to normal levels, you can proceed with your regular meal plan.
2. Treating Severe Hypoglycemia
For individuals who are unable to treat their hypoglycemia due to severe symptoms (such as confusion, loss of consciousness, or inability to swallow), a glucagon injection may be needed. Glucagon is a hormone that triggers the liver to release glucose into the bloodstream. Glucagon injections are often prescribed to people with diabetes who are at risk of severe hypoglycemia.
If someone around you is experiencing severe hypoglycemia, it’s important to seek medical help immediately and, if available, administer the glucagon injection as directed. Emergency medical personnel will provide additional treatment if necessary.
Preventing Low Blood Sugar
Preventing low blood sugar is crucial for individuals with diabetes, especially those taking insulin or medications that increase insulin production. Here are some strategies to reduce the risk of hypoglycemia:
Monitor your blood sugar regularly: Regular blood sugar testing is essential to understanding how your body responds to food, exercise, and medication. This helps you anticipate and prevent drops in blood sugar.
Adjust insulin doses appropriately: Work with your healthcare provider to adjust your insulin doses to account for factors such as meal size, exercise, and stress.
Balance meals and snacks: Ensure that your meals contain a good balance of carbohydrates, protein, and healthy fats to help maintain stable blood sugar levels throughout the day.
Carry a source of fast-acting carbohydrates: Always carry glucose tablets or a sugary snack with you in case you experience symptoms of hypoglycemia when away from home.
Be cautious with alcohol: If you consume alcohol, do so in moderation and always with food to reduce the risk of hypoglycemia.
Stay hydrated: Drink plenty of water to help prevent dehydration, which can affect your blood sugar regulation.
Conclusion
Hypoglycemia is a common concern for people with diabetes, particularly those who use insulin or certain medications to manage their blood sugar. Recognizing the signs and symptoms of low blood sugar, knowing how to manage it, and taking steps to prevent it are essential components of effective diabetes management.
By learning to identify the early warning signs of hypoglycemia and responding quickly, individuals with diabetes can prevent the progression to more severe symptoms and maintain better control over their blood sugar levels. Regular blood sugar monitoring, proper meal planning, and an individualized treatment plan are key to managing low blood sugar and ensuring overall health and well-being. Always consult with your healthcare provider to ensure that your diabetes management plan is tailored to your specific needs.
Related topics:
What Is the Best Reading for Blood Sugar?