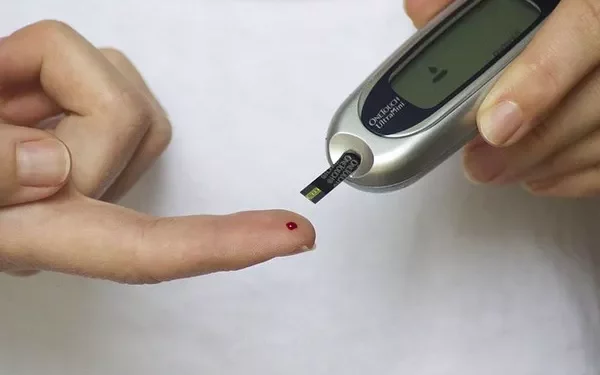
Monitoring blood sugar levels is an essential part of managing diabetes, ensuring that individuals maintain good control over their condition. Understanding what constitutes a healthy blood sugar reading is crucial not only for those diagnosed with diabetes but also for individuals at risk of developing the condition. This article will explore the best readings for blood sugar, detailing what normal, prediabetic, and diabetic blood glucose levels are, as well as how to interpret various measurements for optimal health.
The Importance of Blood Sugar Monitoring
Blood sugar, or blood glucose, is the primary source of energy for the body’s cells. The body regulates blood sugar levels through the hormone insulin, which helps glucose enter cells to be used for energy. However, in people with diabetes, insulin function is impaired, leading to fluctuations in blood glucose levels.
Chronic high blood sugar (hyperglycemia) can lead to a variety of complications, including damage to the eyes, kidneys, heart, and nerves. Conversely, very low blood sugar (hypoglycemia) can cause symptoms such as dizziness, confusion, and even loss of consciousness. Therefore, maintaining blood glucose levels within a healthy range is vital to prevent these complications.
Blood sugar monitoring is crucial for:
- Diagnosing diabetes and prediabetes
- Managing blood glucose levels
- Adjusting medications or insulin doses
- Identifying patterns and trends in glucose levels
- Preventing complications related to high or low blood sugar
Understanding the target blood sugar range and how to achieve it through diet, exercise, medication, and lifestyle changes is essential for overall health and wellness.
The Different Measurements of Blood Sugar
To better understand what constitutes a “good” or “healthy” blood sugar reading, it’s important to familiarize yourself with the different types of blood sugar tests used to monitor and diagnose diabetes. These include:
Fasting Blood Sugar (FBS): This test measures blood sugar after an overnight fast, usually done after at least 8 hours without eating.
Postprandial Blood Sugar (PPBS): This test measures blood sugar levels 1 to 2 hours after a meal. It provides insight into how the body handles glucose after eating.
Oral Glucose Tolerance Test (OGTT): This test involves drinking a glucose solution and having blood sugar levels measured at regular intervals afterward. It helps diagnose prediabetes and type 2 diabetes.
Hemoglobin A1c (HbA1c): This test measures the average blood sugar levels over the past 2 to 3 months by looking at the percentage of hemoglobin in the blood that is coated with sugar (glycated hemoglobin). It provides a long-term view of blood sugar control.
Random Blood Sugar Test: This test measures blood sugar levels at any time of the day, regardless of when the person last ate. It is typically used to diagnose diabetes when symptoms are present.
Each of these tests has different target ranges, and understanding these will help individuals make informed decisions about their health.
Target Blood Sugar Levels: What Is Considered “Normal”?
Understanding what constitutes a healthy blood sugar level is essential for anyone with or at risk for diabetes. While individual needs may vary, medical guidelines provide general ranges for normal, prediabetic, and diabetic blood sugar levels.
1. Fasting Blood Sugar (FBS)
The fasting blood sugar test is typically used to assess how well the body regulates glucose after a period of fasting. The results are typically expressed in milligrams per deciliter (mg/dL).
Normal: A fasting blood sugar level of 70-99 mg/dL is considered normal.
Prediabetes: A fasting blood sugar level of 100-125 mg/dL is considered prediabetic (impaired fasting glucose).
Diabetes: A fasting blood sugar level of 126 mg/dL or higher, confirmed on at least two separate occasions, indicates diabetes.
It is important to note that even if your fasting blood sugar is within the normal range, fluctuations throughout the day can still occur, especially after meals. Therefore, additional testing is often needed to get a comprehensive picture of your blood glucose control.
2. Postprandial Blood Sugar (PPBS)
Postprandial blood sugar is measured 1 to 2 hours after a meal. This test provides insight into how the body processes glucose after food intake and is particularly useful for assessing how well a person’s insulin is working.
Normal: A normal postprandial blood sugar level should be less than 140 mg/dL.
Prediabetes: A postprandial blood sugar level of 140-199 mg/dL suggests prediabetes (impaired glucose tolerance).
Diabetes: A postprandial blood sugar level of 200 mg/dL or higher indicates diabetes.
After eating, blood sugar levels naturally rise due to the absorption of glucose from food. However, in healthy individuals, insulin works to bring blood glucose levels back down within a few hours. In people with diabetes, this process is impaired, leading to prolonged elevated blood glucose levels.
3. Hemoglobin A1c (HbA1c)
The hemoglobin A1c test is a widely used tool to measure long-term blood sugar control. It gives an estimate of the average blood glucose levels over the past 2 to 3 months by evaluating the percentage of hemoglobin molecules that have glucose attached to them.
Normal: An HbA1c level below 5.7% is considered normal.
Prediabetes: An HbA1c level between 5.7% and 6.4% indicates prediabetes.
Diabetes: An HbA1c level of 6.5% or higher on two separate occasions is used to diagnose diabetes.
The HbA1c test is valuable because it provides a longer-term view of how well an individual’s blood glucose levels have been controlled, helping to identify trends and make adjustments to diet, medication, or lifestyle.
4. Oral Glucose Tolerance Test (OGTT)
The OGTT measures how the body responds to a standardized amount of glucose after fasting and drinking a glucose solution. It is typically used to diagnose prediabetes or gestational diabetes.
Normal: A blood glucose level of less than 140 mg/dL two hours after drinking the glucose solution is considered normal.
Prediabetes: A blood glucose level between 140-199 mg/dL two hours after the glucose solution indicates prediabetes (impaired glucose tolerance).
Diabetes: A blood glucose level of 200 mg/dL or higher after the OGTT is considered diagnostic of diabetes.
While the OGTT is particularly helpful for diagnosing diabetes and prediabetes, it can be cumbersome, requiring multiple blood tests, and is not as commonly used as fasting blood sugar or HbA1c tests for routine monitoring.
5. Random Blood Sugar Test
A random blood sugar test is typically used in emergency settings or when symptoms of high blood sugar are present. This test measures blood sugar at any time of the day, regardless of when you last ate.
Normal: There is no strict normal range for a random blood sugar test, but it should generally be less than 140 mg/dL.
Diabetes: A random blood sugar level of 200 mg/dL or higher, especially with symptoms of hyperglycemia (e.g., increased thirst, frequent urination, blurred vision), suggests diabetes.
What Is the Ideal Blood Sugar Reading?
The “best” reading for blood sugar is a target that is as close to normal as possible, but it will depend on individual circumstances. A healthy blood sugar level allows individuals to avoid the complications of both high and low blood sugar while feeling well.
The American Diabetes Association (ADA) provides the following guidelines for target blood sugar levels for most adults with diabetes:
Fasting or Before Meals (preprandial): 80-130 mg/dL
Postprandial (2 hours after meals): Less than 180 mg/dL
Hemoglobin A1c: Less than 7%
These targets may vary depending on the individual’s age, type of diabetes, duration of the condition, and other health factors. For example, older adults or those with significant health complications may have more relaxed blood sugar targets, while younger individuals with newly diagnosed diabetes may have stricter targets.
How to Achieve the Best Blood Sugar Readings
Achieving optimal blood sugar levels involves a combination of healthy lifestyle practices, including:
Diet: Focus on a balanced diet rich in fiber, healthy fats, lean proteins, and low-glycemic carbohydrates. Monitoring carbohydrate intake, especially during meals, can help control blood glucose spikes.
Exercise: Regular physical activity helps increase insulin sensitivity, allowing the body to better use glucose for energy.
Medication: For those with diabetes, medications like oral hypoglycemics or insulin injections may be necessary to keep blood glucose levels in check.
Monitoring: Regular blood sugar monitoring helps individuals understand how their lifestyle, diet, and medications affect their glucose levels, making it easier to make adjustments as needed.
Conclusion
While there is no one-size-fits-all answer for the “best” blood sugar reading, maintaining blood glucose levels within target ranges is crucial for managing diabetes and preventing long-term complications. Healthy blood sugar levels are typically in the range of 70-130 mg/dL before meals and less than 180 mg/dL after meals. Regular blood sugar monitoring and the appropriate use of medications, combined with a healthy lifestyle, can help individuals with diabetes achieve these target levels and improve their quality of life. By working closely with healthcare providers, individuals can develop a personalized plan to keep their blood sugar levels in check and live a healthy, active life.
Related topics:
What are the Best Blood Sugar Monitors