Prediabetes is a condition characterized by higher-than-normal blood sugar levels, but not high enough to be classified as type 2 diabetes. It is a warning sign that the body is beginning to have difficulty regulating blood glucose, a crucial factor in the development of type 2 diabetes. Although prediabetes is often asymptomatic, its early detection is critical, as it can be reversed with appropriate lifestyle changes and medical intervention. This article aims to provide an in-depth understanding of blood sugar levels, what qualifies as prediabetes, how it is diagnosed, and the implications for long-term health.
Understanding Blood Sugar and Its Regulation
Blood sugar (glucose) is the primary source of energy for the body’s cells. It is derived from the food we eat, particularly carbohydrates, which are broken down into glucose and absorbed into the bloodstream. To keep blood glucose levels stable, the body relies on insulin, a hormone produced by the pancreas. Insulin helps move glucose from the bloodstream into the cells, where it is used for energy or stored for future use.
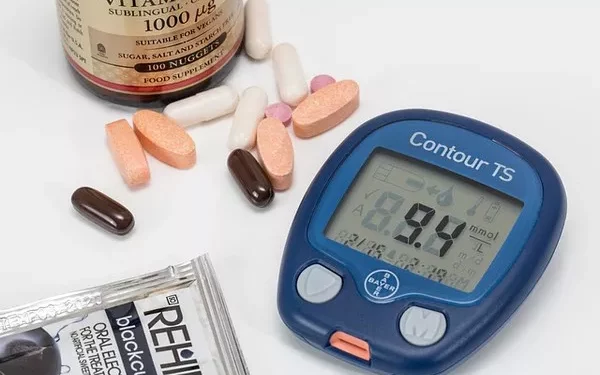
In a healthy individual, blood sugar levels remain within a certain range throughout the day, fluctuating depending on food intake, physical activity, and other factors. However, when the body cannot regulate blood sugar properly, it can lead to conditions like prediabetes and type 2 diabetes. Monitoring blood sugar levels is key to detecting these conditions early and preventing the complications that can arise from chronic high blood sugar.
What is Prediabetes?
Prediabetes is a condition where blood glucose levels are higher than normal, but not yet high enough to meet the criteria for type 2 diabetes. Individuals with prediabetes are at an increased risk of developing type 2 diabetes, heart disease, and stroke. The progression from prediabetes to type 2 diabetes can often be prevented or delayed through lifestyle changes such as diet, exercise, and weight loss.
It is important to note that prediabetes typically does not have any obvious symptoms, so many people may have it without realizing it. Without intervention, however, prediabetes can progress to type 2 diabetes over time, which can result in serious health complications, including nerve damage, kidney disease, vision problems, and cardiovascular disease.
Blood Sugar Levels and Prediabetes Diagnosis
Blood sugar levels are measured using different tests, including fasting blood glucose tests, oral glucose tolerance tests, and hemoglobin A1c tests. These tests help determine where an individual’s blood sugar levels fall within the normal, prediabetic, or diabetic range.
1. Fasting Blood Glucose Test
A fasting blood glucose test measures the level of glucose in the blood after fasting for at least eight hours. It is commonly used to diagnose prediabetes and diabetes. The following ranges are used to interpret the results:
Normal: Fasting blood glucose levels of less than 100 milligrams per deciliter (mg/dL).
Prediabetes: Fasting blood glucose levels between 100 and 125 mg/dL.
Diabetes: Fasting blood glucose levels of 126 mg/dL or higher on two separate occasions.
A fasting blood glucose test is one of the most commonly used methods for diagnosing prediabetes and diabetes. However, a single elevated reading is not enough for a diagnosis; further testing may be required to confirm the results.
2. Oral Glucose Tolerance Test (OGTT)
The OGTT is used to assess how the body processes glucose. It involves drinking a sugary solution after fasting overnight, followed by blood tests at various intervals to measure how the glucose is metabolized over time. This test is often used when the results from other tests are unclear. The following ranges are used to interpret the results of the OGTT:
Normal: Blood glucose levels of less than 140 mg/dL two hours after drinking the glucose solution.
Prediabetes: Blood glucose levels between 140 and 199 mg/dL two hours after drinking the glucose solution.
Diabetes: Blood glucose levels of 200 mg/dL or higher two hours after drinking the glucose solution.
The OGTT is a more sensitive test than the fasting blood glucose test and can detect abnormalities in glucose metabolism that may not be detected otherwise.
3. Hemoglobin A1c Test
The hemoglobin A1c test measures the average blood sugar levels over the past two to three months. It is a useful tool for assessing long-term blood glucose control. The following ranges are used to interpret the results of the A1c test:
Normal: A1c levels of less than 5.7%.
Prediabetes: A1c levels between 5.7% and 6.4%.
Diabetes: A1c levels of 6.5% or higher.
The A1c test is often used for the diagnosis of prediabetes and diabetes, as well as for monitoring long-term blood glucose control in individuals with diabetes.
Causes and Risk Factors for Prediabetes
Prediabetes occurs when the body becomes resistant to insulin or when the pancreas cannot produce enough insulin to maintain normal blood sugar levels. As a result, glucose builds up in the bloodstream instead of being absorbed by the cells. While the exact cause of prediabetes is not fully understood, several factors can increase the risk of developing the condition.
1. Obesity and Overweight
Excess body weight, particularly abdominal fat, is a major risk factor for prediabetes. Fat cells release hormones and other substances that can impair the body’s ability to use insulin effectively, leading to insulin resistance. Losing even a small amount of weight through diet and exercise can significantly reduce the risk of developing prediabetes.
2. Sedentary Lifestyle
Physical inactivity is another key risk factor for prediabetes. Regular physical activity helps improve insulin sensitivity, meaning the body’s cells become more responsive to insulin. Lack of exercise can lead to insulin resistance, which increases the likelihood of developing prediabetes.
3. Age
The risk of developing prediabetes increases with age. While prediabetes can occur at any age, people over 45 are more likely to develop the condition. As we age, our bodies may become less efficient at regulating blood sugar, increasing the likelihood of insulin resistance.
4. Family History
Having a family history of diabetes increases the risk of developing prediabetes. If a parent or sibling has type 2 diabetes, your chances of developing the condition are higher due to genetic factors.
5. Ethnicity
Certain ethnic groups are at higher risk for prediabetes and type 2 diabetes. These include African Americans, Hispanic Americans, Native Americans, and Asian Americans. Genetic and environmental factors may contribute to this increased risk.
6. Gestational Diabetes
Women who have had gestational diabetes during pregnancy are at increased risk of developing prediabetes or type 2 diabetes later in life. Gestational diabetes occurs when a woman’s blood sugar levels become too high during pregnancy, and it increases the likelihood of insulin resistance after childbirth.
7. High Blood Pressure and Cholesterol Levels
High blood pressure (hypertension) and abnormal cholesterol levels are common in people with prediabetes. Both conditions are risk factors for the development of cardiovascular disease and can increase the likelihood of developing type 2 diabetes.
8. Polycystic Ovary Syndrome (PCOS)
Women with polycystic ovary syndrome (PCOS) are at higher risk of developing prediabetes due to hormonal imbalances that can affect insulin sensitivity. PCOS is characterized by irregular menstrual cycles, elevated levels of male hormones, and the development of cysts on the ovaries.
Symptoms of Prediabetes
One of the biggest challenges of prediabetes is that it often does not present with any noticeable symptoms. Most people with prediabetes do not experience any signs or symptoms until their blood sugar levels reach the diabetic range. However, some individuals may notice subtle signs that could indicate elevated blood sugar levels, such as:
- Increased thirst
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing cuts or sores
- Dark patches of skin, particularly around the neck or armpits (a condition called acanthosis nigricans)
If you experience any of these symptoms, it is important to consult with a healthcare provider and undergo blood sugar testing.
Preventing and Managing Prediabetes
While prediabetes is a serious health condition, it is important to know that it is reversible with lifestyle changes. By making healthy choices, individuals with prediabetes can prevent or delay the onset of type 2 diabetes.
1. Dietary Modifications
A healthy, balanced diet is critical for managing blood sugar levels and improving insulin sensitivity. Focus on eating whole, nutrient-dense foods, such as:
Non-starchy vegetables: Leafy greens, broccoli, cauliflower, and peppers
Whole grains: Oats, quinoa, brown rice, and barley
Lean proteins: Chicken, fish, beans, and legumes
Healthy fats: Avocados, nuts, seeds, and olive oil
Avoid foods high in refined carbohydrates, added sugars, and unhealthy fats, such as sugary drinks, processed snacks, and fried foods.
2. Regular Physical Activity
Engaging in regular physical activity can help improve insulin sensitivity and promote weight loss. Aim for at least 150 minutes of moderate-intensity aerobic activity (e.g., brisk walking) per week, along with strength training exercises twice a week.
3. Weight Loss
Losing excess weight can help improve insulin sensitivity and reduce the risk of developing type 2 diabetes. Even a modest weight loss of 5-10% of body weight can have significant health benefits.
4. Regular Monitoring
If you have been diagnosed with prediabetes, it is important to monitor your blood sugar levels regularly. Your healthcare provider may recommend routine blood tests, including fasting blood glucose and hemoglobin A1c tests, to track your progress and ensure that your blood sugar levels remain within a healthy range.
5. Medication
In some cases, medication may be prescribed to help manage blood sugar levels. The most common medication for prediabetes is metformin, which helps lower blood glucose levels by improving insulin sensitivity. However, lifestyle changes should still be the primary approach for managing prediabetes.
Conclusion
Prediabetes is a critical stage in the development of type 2 diabetes, but with early detection and appropriate lifestyle changes, it is possible to reverse the condition and prevent the onset of diabetes. Monitoring blood sugar levels, understanding what constitutes prediabetes, and making dietary, exercise, and lifestyle modifications can help individuals with prediabetes regain control over their health. By taking proactive steps today, individuals with prediabetes can significantly reduce their risk of developing type 2 diabetes and improve their long-term health outcomes.
Related topics:
What Range Should Blood Sugar Levels Be Kept In