Monitoring blood sugar levels is a critical aspect of managing diabetes, but it is equally important in newborn care. Blood sugar levels in newborns are indicative of their overall health, particularly their metabolic function. Understanding what constitutes a normal blood sugar range for newborns is vital for both parents and healthcare providers to ensure optimal health and prevent complications that may arise from abnormal blood glucose levels.
In this comprehensive article, we will explore the normal blood sugar ranges for newborns, how blood sugar is monitored in neonates, and the risks associated with abnormal blood sugar levels. We will also discuss the factors that influence newborn blood sugar levels, including gestational diabetes, premature birth, and the role of breastfeeding.
Understanding Newborn Blood Sugar
Newborn blood sugar levels differ from those of older children and adults due to the unique physiological processes at birth. The newborn’s body is adapting to life outside the womb, and metabolic regulation is still in its early stages. As a result, blood sugar levels can fluctuate within the first few hours and days of life.
In general, newborns are born with relatively higher blood glucose levels compared to adults. However, their blood sugar levels can drop after birth, particularly in the first few hours as they transition to feeding and using energy independently. For this reason, it is crucial to monitor their blood sugar levels closely during this period to detect any abnormalities that could lead to health complications.
What Is Considered Normal Blood Sugar for Newborns?
Normal blood sugar levels for newborns typically vary based on the age of the infant in hours, their gestational age, and whether they are full-term or premature. However, certain general guidelines can help healthcare providers determine if a newborn’s blood sugar levels fall within a safe range.
At birth (0 to 1 hour after birth): Blood sugar levels in newborns typically range between 50-100 mg/dL (2.8-5.6 mmol/L). The body’s glucose reserves and hormones help stabilize blood sugar levels in the first few hours after birth.
1 to 2 hours after birth: A typical blood sugar range at this time is between 45-90 mg/dL (2.5-5.0 mmol/L).
After the first 24 hours: Blood sugar levels generally stabilize and can range from 50-80 mg/dL (2.8-4.4 mmol/L).
It is important to note that newborns who are premature or have specific medical conditions may have slightly different blood sugar targets. Additionally, hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar) are concerns for some newborns and may require specific interventions.
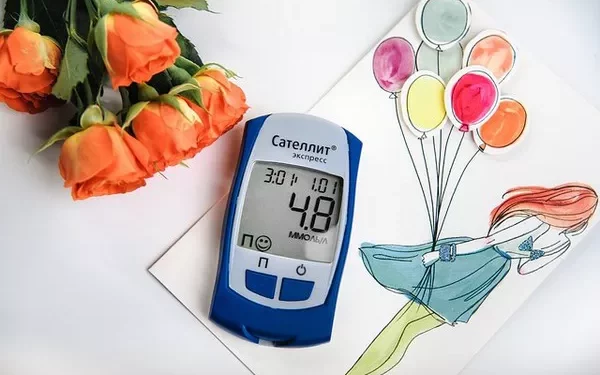
Blood Sugar Monitoring in Newborns
Monitoring blood sugar in newborns is essential, especially in the first few hours and days of life when the baby is adjusting to extrauterine life. For full-term babies, blood sugar monitoring is often conducted in the first 2 to 4 hours after birth to ensure that glucose levels stabilize.
Blood glucose is typically measured using a heel stick test to collect blood for a glucose test or through a continuous glucose monitoring system if there is an ongoing concern. If a newborn has any risk factors for abnormal blood sugar levels (discussed below), healthcare providers may monitor blood sugar more frequently.
Signs of Low Blood Sugar in Newborns
Low blood sugar, or neonatal hypoglycemia, can occur when the baby does not have enough glucose in their bloodstream to meet their energy needs. Newborns can experience hypoglycemia for various reasons, and it is essential to recognize the symptoms early.
Symptoms of low blood sugar in newborns include:
- Jitteriness or tremors
- Poor feeding or difficulty sucking
- Lethargy or difficulty staying awake
- Fluctuating body temperature (hypothermia)
- Pale or blue skin tone
- Rapid breathing or irregular breathing patterns
- Seizures (in severe cases)
In these cases, immediate intervention is necessary to raise the baby’s blood sugar levels and avoid further complications.
Signs of High Blood Sugar in Newborns
On the opposite end of the spectrum, hyperglycemia, or high blood sugar, is less common in healthy newborns but may occur in certain conditions such as gestational diabetes or infections. The symptoms of high blood sugar in newborns are more subtle but still important to watch for.
Signs of high blood sugar in newborns include:
- Excessive thirst or dehydration
- Frequent urination
- Rapid breathing or breathing difficulty
- Poor feeding or lethargy
- Unexplained weight loss
If a newborn’s blood sugar is found to be consistently high, it may be a sign of a more significant underlying issue, such as neonatal diabetes, and prompt medical evaluation is necessary.
Factors Affecting Newborn Blood Sugar Levels
A number of factors can affect a newborn’s blood sugar levels, both positively and negatively. These factors can be influenced by the baby’s overall health, gestational age, and environment.
1. Gestational Diabetes in the Mother
One of the primary risk factors for abnormal blood sugar levels in newborns is gestational diabetes (GDM) in the mother. Gestational diabetes occurs when a pregnant woman develops high blood sugar levels, typically in the second or third trimester, due to insulin resistance. Babies born to mothers with gestational diabetes are at higher risk for experiencing neonatal hypoglycemia after birth.
This is because the baby’s pancreas may produce more insulin to deal with the elevated blood sugar levels in utero. However, after birth, the baby’s insulin production may remain elevated, leading to low blood sugar levels as the supply of glucose from the placenta ceases.
2. Premature Birth
Premature infants, especially those born before 32 weeks of gestation, are at a higher risk for hypoglycemia because their liver may not yet be capable of storing enough glucose. Premature infants also have lower fat reserves and reduced ability to regulate their blood sugar levels effectively.
Because of these factors, premature newborns are more likely to require closer monitoring and potentially glucose supplementation to stabilize their blood sugar levels in the first few days of life.
3. Low Birth Weight and Small for Gestational Age (SGA) Babies
Low birth weight (less than 5.5 pounds or 2.5 kilograms) and babies who are small for their gestational age (SGA) are also at an increased risk for low blood sugar after birth. These babies may have reduced glycogen stores, which can result in more significant fluctuations in blood sugar during the first few hours of life.
4. Infections or Illness
Infections or illness during birth can interfere with the baby’s metabolic processes, leading to unstable blood sugar levels. For example, if a newborn develops a systemic infection, their blood sugar may rise as part of the body’s stress response. Conversely, illnesses that affect the digestive system, such as jaundice, can hinder the baby’s ability to feed effectively and contribute to low blood sugar levels.
5. Feeding and Breastfeeding
Feeding practices play a vital role in maintaining normal blood sugar levels in newborns. Glucose is a primary source of energy for infants, and providing the newborn with adequate nutrition is essential for stabilizing their blood sugar levels.
Breastfeeding is ideal because breast milk contains natural sugars that help maintain normal glucose levels. In cases where breastfeeding is not possible, infant formula can provide an alternative source of glucose. However, if a newborn is not feeding well, blood sugar levels may drop, and intervention (such as glucose supplementation or IV fluids) may be necessary to stabilize their blood sugar.
6. Birth Stress or Complications
Stress during birth, whether due to a prolonged labor, delivery complications, or the need for interventions such as a cesarean section, can influence a newborn’s blood sugar levels. These stressors may cause temporary elevations in blood sugar or contribute to hypoglycemia after birth as the baby’s stress hormone levels normalize.
Managing and Correcting Abnormal Blood Sugar in Newborns
If a newborn is diagnosed with abnormal blood sugar levels, timely intervention is critical to avoid complications. The treatment approach will depend on the severity of the hypoglycemia or hyperglycemia and the underlying causes.
Hypoglycemia Treatment
For mild cases of neonatal hypoglycemia (blood sugar levels slightly below the normal range), the baby may simply need to be fed more frequently, either by breastfeeding or formula feeding. In some cases, a small amount of glucose may be given orally.
For more severe cases, where blood sugar levels drop significantly, intravenous (IV) glucose may be necessary to raise the blood sugar levels quickly. In extremely rare cases, if a newborn’s blood sugar does not respond to initial interventions, further testing and medical management may be required.
Hyperglycemia Treatment
In cases of neonatal hyperglycemia, treatment focuses on identifying and managing the underlying cause. If the hyperglycemia is related to stress, infection, or another temporary condition, blood sugar levels typically stabilize once the underlying issue is treated. In rare cases, medication may be necessary to lower blood sugar levels if they remain elevated for an extended period.
Conclusion
Monitoring blood sugar levels in newborns is a critical aspect of ensuring their health and well-being, especially in the early hours and days of life when their bodies are adjusting to new metabolic processes. The ideal blood sugar range for newborns generally falls between 50-100 mg/dL (2.8-5.6 mmol/L) in the first few hours after birth, stabilizing over time.
Abnormal blood sugar levels, whether low or high, can be indicative of underlying health issues such as prematurity, gestational diabetes, or infections. Early detection and appropriate intervention can prevent complications and help ensure that newborns have the best start in life.
Parents and healthcare providers should be vigilant about monitoring blood sugar levels in newborns, especially those at higher risk, to prevent long-term health issues. Early and effective management of abnormal blood sugar levels can contribute to the overall health and development of the baby, allowing for a healthy transition to life outside the womb.
Related topics:
What Constitutes a Normal Healthy Blood Sugar Level