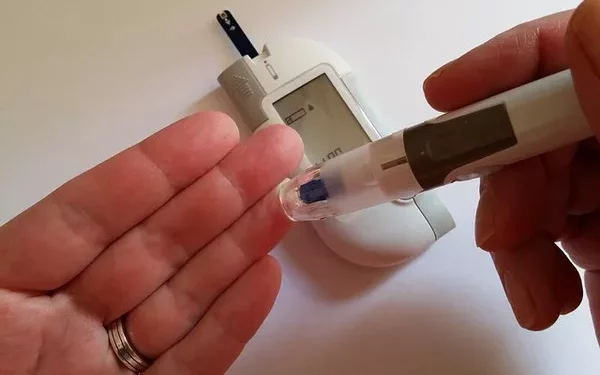
Blood sugar monitoring is a vital aspect of diabetes management, allowing individuals to track their glucose levels and make informed lifestyle and treatment decisions. However, the optimal frequency for checking blood sugar varies widely based on factors such as diabetes type, treatment regimen, lifestyle, and personal health goals. This article explores the ideal blood sugar testing frequency for various scenarios, discussing how often to test, why it matters, and how to tailor testing to individual needs.
Understanding Blood Sugar Monitoring
Monitoring blood sugar, also known as blood glucose testing, helps people with diabetes maintain target glucose levels. Regular testing can:
Prevent hyperglycemia and hypoglycemia: Frequent testing helps catch high or low blood sugar early, preventing serious complications.
Guide medication and insulin dosing: Accurate blood sugar readings inform insulin or medication adjustments, optimizing control.
Support dietary and lifestyle decisions: Testing before and after meals helps individuals understand how foods impact their glucose, allowing more precise dietary choices.
Provide valuable data for healthcare providers: Consistent blood sugar records enable healthcare providers to adjust treatment plans as needed, improving long-term outcomes.
How Many Times a Day Should You Check Your Blood Sugar?
There’s no universal rule for how often to check blood sugar; it varies based on diabetes type, treatment, individual goals, and health circumstances. Below are guidelines for common diabetes management scenarios:
1. Type 1 Diabetes
People with type 1 diabetes often need to check their blood sugar multiple times daily due to the lack of natural insulin production. Testing is critical in managing insulin dosing and avoiding extreme blood sugar fluctuations.
Recommended Testing Frequency:
Upon Waking: A fasting blood sugar test helps establish a baseline for the day.
Before Meals: Testing before each meal helps determine the insulin dose needed.
2 Hours After Meals: Post-meal testing shows how the meal and insulin affected blood sugar, helping fine-tune future insulin dosages.
Before Bedtime: Testing before bed helps ensure safe glucose levels overnight.
During Physical Activity: Checking before, during, and after exercise can prevent hypoglycemia.
If Feeling Unwell: Illness or stress can impact blood sugar, so additional checks may be needed.
Average Testing Frequency: 6–10 times per day.
2. Type 2 Diabetes with Insulin Therapy
Type 2 diabetes patients on insulin therapy, especially those taking rapid-acting or multiple daily insulin injections, often benefit from frequent blood sugar testing. The exact number of checks varies based on individual needs and the type of insulin regimen.
Recommended Testing Frequency:
Upon Waking: Provides baseline fasting glucose.
Before and After Meals: Helps manage insulin doses and track the effects of food.
Before Bedtime: Ensures glucose is stable for the night.
During Physical Activity: To avoid hypoglycemia if using rapid-acting insulin.
If Experiencing Symptoms of High or Low Blood Sugar: Allows for immediate corrective action.
Average Testing Frequency: 4–8 times per day.
3. Type 2 Diabetes with Oral Medications
For individuals with type 2 diabetes managed with oral medications and lifestyle changes, blood sugar monitoring frequency may be less intensive. Still, regular testing can provide valuable insights into blood sugar trends and guide medication and lifestyle adjustments.
Recommended Testing Frequency:
Upon Waking: Fasting blood sugar provides an essential baseline.
Occasionally Before and After Meals: Testing around meals helps identify foods that may cause spikes.
Occasionally Before Bed: Pre-bedtime testing can provide insights into glucose stability overnight.
Average Testing Frequency: 1–4 times per day, depending on individual circumstances.
4. Gestational Diabetes
Pregnant women with gestational diabetes need to monitor blood sugar closely to protect both their health and the baby’s development. Testing frequency is typically higher due to the rapid changes in glucose levels during pregnancy.
Recommended Testing Frequency:
Upon Waking: Establishes fasting blood sugar levels.
Before and After Meals: Ensures that blood sugar levels are within the recommended range after eating.
Before Bedtime: Helps ensure stable blood sugar overnight.
Average Testing Frequency: 4–7 times per day.
5. Intensive Insulin Therapy or Insulin Pump Users
Individuals on intensive insulin therapy, including those using an insulin pump, generally require frequent blood sugar checks to fine-tune their therapy and adjust insulin doses accurately. Since insulin pumps deliver continuous doses, precise monitoring is essential for effective blood sugar control.
Recommended Testing Frequency:
Upon Waking and Before Bed: Establishes a baseline and nighttime safety.
Before and After Meals: To adjust bolus insulin dosing.
During and After Exercise: To avoid hypoglycemia or hyperglycemia.
If Experiencing Symptoms of Hyperglycemia or Hypoglycemia: For immediate correction.
Frequent Monitoring Throughout the Day: Helps optimize pump settings and prevent unexpected fluctuations.
Average Testing Frequency: 8–12 times per day.
Factors Influencing Blood Sugar Monitoring Frequency
In addition to diabetes type and treatment regimen, several factors influence how often a person should test their blood sugar:
Health Status: Illness, stress, or hormonal changes can impact blood sugar levels. People experiencing these factors may need to increase their testing frequency temporarily.
Lifestyle: Changes in diet, exercise, and routine can affect blood sugar. For example, starting a new exercise program or changing eating patterns might require more frequent testing initially.
Medication Adjustments: Adjusting insulin or other diabetes medications may require temporary increases in testing frequency to monitor effects on blood sugar.
Blood Sugar Targets: Individuals with tighter blood sugar targets may test more frequently to stay within their goal range.
Personal Comfort: Some people feel more secure testing frequently, while others prefer to test less often. Finding a balance that provides necessary information without causing stress is essential.
Continuous Glucose Monitoring (CGM): An Alternative to Frequent Testing
Continuous glucose monitoring (CGM) has become an essential tool for many people with diabetes, offering real-time glucose readings and trends. CGM devices measure interstitial glucose levels every few minutes, providing a continuous picture of blood sugar trends. This technology is especially useful for:
Reducing the Frequency of Fingerstick Tests: While CGM doesn’t entirely replace fingerstick tests, it reduces the need for frequent checks.
Early Detection of Blood Sugar Trends: CGM alerts users to rising or falling glucose, allowing for faster corrective action.
Improving Blood Sugar Control: With continuous feedback, CGM users can make more informed decisions regarding food, exercise, and insulin dosing.
CGM is most beneficial for people with type 1 diabetes or those on intensive insulin therapy, but it may also benefit individuals with type 2 diabetes requiring frequent monitoring.
Practical Tips for Effective Blood Sugar Monitoring
For accurate and practical blood sugar monitoring, consider the following tips:
Maintain a Routine: Testing at consistent times, like before meals and at bedtime, provides valuable trend data.
Log Your Results: Keeping a record of your blood sugar readings, along with notes on food, activity, and any unusual symptoms, helps identify patterns.
Stay Hydrated: Dehydration can affect blood sugar levels and lead to inaccurate readings.
Clean Hands: Always wash hands before testing to avoid contamination that could skew results.
Rotate Testing Sites: Regularly changing the testing site on your finger can reduce soreness.
Consulting Your Healthcare Provider for Personalized Guidance
Your healthcare provider is an invaluable resource in determining the right blood sugar testing frequency for your unique situation. They can analyze your data, recommend adjustments, and provide guidance tailored to your health needs and diabetes management goals.
Conclusion
The optimal frequency for blood sugar monitoring depends on numerous factors, including the type of diabetes, treatment plan, lifestyle, and individual health goals. While individuals with type 1 diabetes or those on intensive insulin therapy may need to check their blood sugar up to 10 times a day, people with type 2 diabetes on oral medications may only need to test a few times a week.
Continuous glucose monitoring technology has revolutionized blood sugar tracking, offering convenience and comprehensive data that help people make informed choices. Ultimately, the key to successful diabetes management lies in finding a monitoring routine that aligns with your treatment plan and personal preferences, helping you achieve better blood sugar control and improved quality of life.
Related topics:
How to Check Blood Sugar Without Sticking Finger