Hyperglycemia, or high blood glucose levels, is a hallmark of both type 1 and type 2 diabetes. When blood sugar levels remain elevated over time, they can cause widespread damage to various organs and systems in the body. Among the most critical targets of hyperglycemia are the blood vessels, which play a vital role in supplying oxygen and nutrients to tissues throughout the body. Chronic hyperglycemia leads to a process called “vascular complications,” which significantly increases the risk of conditions such as heart disease, stroke, kidney failure, blindness, and peripheral artery disease.
This article will delve into how hyperglycemia damages blood vessels, the underlying mechanisms, the consequences of this damage, and what can be done to prevent or mitigate vascular complications in people with diabetes.
The Importance of Blood Vessels in the Body
Blood vessels are the highways of the body, responsible for transporting essential substances such as oxygen, nutrients, hormones, and immune cells to tissues. They are classified into two main types:
Microvasculature (small vessels): These include capillaries, arterioles, and venules. They are responsible for the direct exchange of substances between blood and tissues.
Macrovasculature (large vessels): These include arteries and veins, which carry blood to and from major organs and the rest of the body.
In a healthy body, the walls of blood vessels are flexible and smooth, allowing for proper blood flow and the delivery of vital substances to tissues. Hyperglycemia, however, disrupts these normal functions, leading to damage to both small and large blood vessels.
Mechanisms of Blood Vessel Damage in Hyperglycemia
The mechanisms by which hyperglycemia damages blood vessels are multifactorial. Here’s an overview of the key processes:
1. Advanced Glycation End Products (AGEs)
One of the main ways hyperglycemia causes blood vessel damage is through the formation of advanced glycation end products (AGEs).
What Are AGEs? AGEs are proteins or lipids that become glycated (bonded with sugar molecules) after being exposed to high levels of glucose over time. In hyperglycemia, the excess glucose in the bloodstream attaches to various proteins in the body, including those in blood vessels.
How Do AGEs Damage Vessels? AGEs can directly alter the structure and function of blood vessels by stiffening their walls and promoting inflammation. When AGEs accumulate in the endothelial cells (the cells lining blood vessels), they impair the vessels’ ability to expand and contract, reducing blood flow and increasing the risk of blockages. AGEs also bind to specific receptors (RAGEs), triggering inflammation and oxidative stress, which further damages the blood vessels.
2. Oxidative Stress and Free Radical Production
Hyperglycemia-Induced Oxidative Stress: Chronic high blood sugar increases the production of reactive oxygen species (ROS), commonly known as free radicals. These are unstable molecules that can damage cells and tissues, including the endothelial cells of blood vessels.
How Oxidative Stress Affects Blood Vessels: In a hyperglycemic environment, excess ROS overwhelms the body’s natural antioxidant defenses, leading to oxidative stress. This oxidative damage disrupts the normal function of blood vessels, causing them to become more permeable, which can result in leakage and swelling. The damage to the vessel walls also promotes the development of atherosclerotic plaques, increasing the risk of cardiovascular complications.
3. Endothelial Dysfunction
The endothelium is the thin layer of cells that lines the inner surface of blood vessels. It plays a critical role in regulating vascular tone (the degree of constriction or dilation of blood vessels), blood flow, and the prevention of blood clotting. Hyperglycemia contributes to endothelial dysfunction, which is one of the earliest indicators of vascular complications.
Mechanisms of Endothelial Dysfunction:
Nitric Oxide (NO) Impairment: Under normal conditions, the endothelium produces nitric oxide, a molecule that relaxes and dilates blood vessels, ensuring smooth blood flow. Hyperglycemia decreases the production of nitric oxide and increases the breakdown of existing NO, leading to vasoconstriction (narrowing of blood vessels) and increased blood pressure.
Pro-inflammatory State: Chronic hyperglycemia induces a pro-inflammatory environment within the endothelium. Elevated levels of cytokines (inflammatory molecules) attract immune cells to the blood vessel walls, which further promotes inflammation, vessel stiffness, and the formation of blood clots.
4. Protein Kinase C (PKC) Activation
Protein kinase C (PKC) is an enzyme that plays a role in various cellular processes, including regulating blood flow, permeability, and cell growth. Hyperglycemia leads to the activation of certain isoforms of PKC, which contribute to vascular damage.
Effects of PKC Activation:
Increased Vascular Permeability: PKC activation increases the permeability of blood vessels, allowing proteins and fluids to leak into surrounding tissues, leading to swelling and tissue damage.
Promotion of Inflammation and Thrombosis: PKC activation also promotes the expression of molecules that encourage inflammation and clot formation, further exacerbating vascular damage and increasing the risk of complications such as heart attacks or strokes.
5. Increased Sorbitol Pathway Activity
The sorbitol pathway, also known as the polyol pathway, is a secondary pathway for glucose metabolism. In hyperglycemia, excess glucose is shunted into this pathway, leading to the accumulation of sorbitol, a sugar alcohol, in cells.
Impact on Blood Vessels:
Osmotic Stress: The accumulation of sorbitol inside endothelial cells creates osmotic stress, drawing water into the cells and causing them to swell and become dysfunctional.
Depletion of NADPH: The sorbitol pathway uses up NADPH, a molecule essential for the regeneration of glutathione, one of the body’s most important antioxidants. This depletion reduces the cells’ ability to defend against oxidative damage, further contributing to vascular injury.
6. Chronic Inflammation
Chronic inflammation is a major consequence of hyperglycemia and plays a central role in blood vessel damage. Elevated blood glucose levels trigger an immune response, with immune cells releasing inflammatory cytokines and promoting the recruitment of more immune cells to the site of vessel damage.
Consequences of Chronic Inflammation:
Atherosclerosis: Inflammation in the blood vessels promotes the formation of atherosclerotic plaques, which are deposits of fat, cholesterol, and other substances that build up on the artery walls. These plaques narrow the blood vessels and restrict blood flow, increasing the risk of heart attacks and strokes.
Endothelial Damage: Prolonged inflammation damages the endothelial cells, impairing their ability to regulate blood pressure, clot formation, and vessel dilation.
Consequences of Blood Vessel Damage in Hyperglycemia
Hyperglycemia-related blood vessel damage can lead to both microvascular and macrovascular complications, which are responsible for many of the long-term health issues associated with diabetes.
1. Microvascular Complications
Diabetic Retinopathy: The tiny blood vessels in the retina (the light-sensitive part of the eye) are particularly vulnerable to hyperglycemia-induced damage. Over time, these vessels can leak, swell, or become blocked, leading to vision problems and, eventually, blindness if untreated.
Diabetic Nephropathy: Hyperglycemia damages the small blood vessels in the kidneys, impairing their ability to filter waste from the blood. This can lead to kidney disease and, in severe cases, kidney failure requiring dialysis or a kidney transplant.
Diabetic Neuropathy: High blood glucose levels damage the small blood vessels that supply nerves, particularly in the extremities. This leads to nerve damage (neuropathy), resulting in symptoms such as numbness, tingling, pain, or weakness, most commonly in the feet and hands.
2. Macrovascular Complications
Coronary Artery Disease (CAD): Damage to the larger blood vessels can lead to coronary artery disease, where the arteries supplying the heart become narrowed or blocked. This increases the risk of heart attacks, heart failure, and other cardiovascular complications.
Peripheral Artery Disease (PAD): Hyperglycemia can damage the large blood vessels that supply blood to the limbs, particularly the legs. This results in reduced blood flow to the extremities, causing pain, slow wound healing, and, in severe cases, the need for amputation.
Cerebrovascular Disease: Damage to the blood vessels supplying the brain can lead to cerebrovascular disease, increasing the risk of strokes and transient ischemic attacks (TIAs), also known as mini-strokes.
Prevention and Management of Hyperglycemia-Induced Vascular Damage
Preventing or minimizing blood vessel damage in people with diabetes requires a multifaceted approach that focuses on maintaining good glycemic control, adopting healthy lifestyle habits, and addressing other risk factors.
1. Glycemic Control
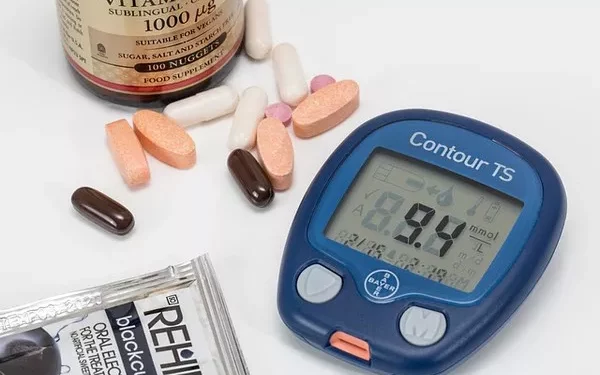
Target Blood Glucose Levels: Keeping blood glucose levels within a target range is the most important strategy for preventing vascular complications. This can be achieved through a combination of medication (such as insulin or oral hypoglycemic agents), regular blood glucose monitoring, and adherence to a diabetes-friendly diet.
HbA1c Monitoring: The HbA1c test provides an indication of average blood glucose levels over the past 2-3 months. Maintaining an HbA1c level below 7% is generally recommended for most people with diabetes to reduce the risk of complications.
2. Blood Pressure and Lipid Management
In addition to controlling blood glucose, managing blood pressure and cholesterol levels is crucial for protecting blood vessels. People with diabetes are often prescribed medications such as statins and ACE inhibitors to help control these factors.
3. Healthy Lifestyle Habits
Diet: A heart-healthy diet that is low in saturated fats, refined carbohydrates, and added sugars can help protect blood vessels and prevent the development of atherosclerosis.
Exercise: Regular physical activity improves blood circulation, reduces blood pressure, and helps regulate blood glucose levels.
Smoking Cessation: Smoking significantly increases the risk of vascular complications in people with diabetes. Quitting smoking is one of the most effective ways to protect blood vessels.
4. Regular Monitoring and Check-Ups
People with diabetes should have regular check-ups with their healthcare providers to monitor for early signs of vascular complications. This includes annual eye exams, kidney function tests, and assessments of nerve function and circulation in the limbs.
See also: What Chromosome is Type 1 Diabetes Found On?
Conclusion
Hyperglycemia poses a serious threat to the integrity of blood vessels, leading to both microvascular and macrovascular complications. The damage is driven by multiple mechanisms, including the formation of AGEs, oxidative stress, endothelial dysfunction, and chronic inflammation. These processes result in a range of complications, from diabetic retinopathy and nephropathy to heart disease and stroke. However, with proper management of blood glucose levels, lifestyle modifications, and medical interventions, it is possible to prevent or delay the onset of vascular complications in people with diabetes.
Related topics:
What Are the Effects of Hypoglycemia?